Procedure
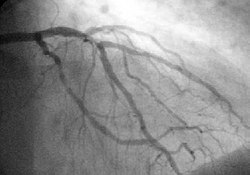
During a protected percutaneous coronary intervention (Protected PCI) procedure, "the Impella 2.5 heart pump helps maintain a stable heart function by pumping blood for the heart. This gives a weak heart muscle an opportunity to rest and reduces the heart’s workload, preventing the heart from being overstressed by the procedure as coronary artery blockages are repaired". [3] Deborah Moore, the Director of Interventional Cardiology at Florida Hospital Zephyrhills, stated that protected PCI is beneficial in patients who are "inoperable or non-candidates for stents and angioplasty." [3] The Impella 2.5, used in protected PCI, "received FDA approval for elective and urgent high-risk PCI procedures in March 2015, following its 510(k) clearance in 2008" and as a percutaneous hemodynamic support device, it was deemed "safe and effective for patients with complex coronary disease, depressed ejection fraction, other co-morbidities, and who have been refused for surgical treatment." [4] The PROTECT II Study, published in Circulation found that the "Impella 2.5 provided superior hemodynamic support in comparison with IABP, with maximal decrease in cardiac power output from baseline of −0.04±0.24 W in comparison with −0.14±0.27 W for IABP (P=0.001)." [5] Hospitals such as Detroit Medical Center, and organizations such as the Society of Cardiovascular Angiography and Interventions, have featured lectures including "The New Era of Protected PCI: Treating Elective and High-Risk PCI Patients with Impella 2.5", [6] and "Expanding your Patient Practice with Protected PCI: Treating the Most Complex Patients" in order to educate physicians on using protected percutaneous coronary intervention, respectively. [7]
This page is based on this
Wikipedia article Text is available under the
CC BY-SA 4.0 license; additional terms may apply.
Images, videos and audio are available under their respective licenses.