Related Research Articles

Beta cells (β-cells) are specialized endocrine cells located within the pancreatic islets of Langerhans responsible for the production and release of insulin and amylin. Constituting ~50–70% of cells in human islets, beta cells play a vital role in maintaining blood glucose levels. Problems with beta cells can lead to disorders such as diabetes.
Hyperinsulinemic hypoglycemia describes the condition and effects of low blood glucose caused by excessive insulin. Hypoglycemia due to excess insulin is the most common type of serious hypoglycemia. It can be due to endogenous or injected insulin.

Congenital hyperinsulinism (HI or CHI) is a rare condition causing severe hypoglycemia in newborns due to the overproduction of insulin. There are various causes of HI, some of which are known to be the result of a genetic mutation. Sometimes HI occurs on its own (isolated) and more rarely associated with other medical conditions.

Diazoxide, sold under the brand name Proglycem and others, is a medication used to treat low blood sugar due to a number of specific causes. This includes islet cell tumors that cannot be removed and leucine sensitivity. It can also be used in refractory cases of sulfonylurea toxicity. It is generally taken by mouth.
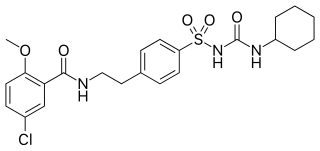
Glibenclamide, also known as glyburide, is an antidiabetic medication used to treat type 2 diabetes. It is recommended that it be taken together with diet and exercise. It may be used with other antidiabetic medication. It is not recommended for use by itself in type 1 diabetes. It is taken by mouth.

Acetohexamide is a first-generation sulfonylurea medication used to treat diabetes mellitus type 2, particularly in people whose diabetes cannot be controlled by diet alone.
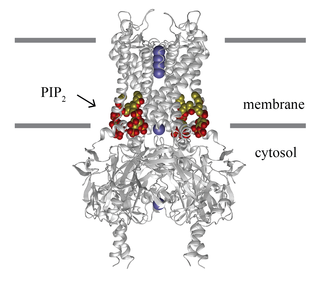
Inward-rectifier potassium channels (Kir, IRK) are a specific lipid-gated subset of potassium channels. To date, seven subfamilies have been identified in various mammalian cell types, plants, and bacteria. They are activated by phosphatidylinositol 4,5-bisphosphate (PIP2). The malfunction of the channels has been implicated in several diseases. IRK channels possess a pore domain, homologous to that of voltage-gated ion channels, and flanking transmembrane segments (TMSs). They may exist in the membrane as homo- or heterooligomers and each monomer possesses between 2 and 4 TMSs. In terms of function, these proteins transport potassium (K+), with a greater tendency for K+ uptake than K+ export. The process of inward-rectification was discovered by Denis Noble in cardiac muscle cells in 1960s and by Richard Adrian and Alan Hodgkin in 1970 in skeletal muscle cells.

GLUD1 is a mitochondrial matrix enzyme, one of the family of glutamate dehydrogenases that are ubiquitous in life, with a key role in nitrogen and glutamate (Glu) metabolism and energy homeostasis. This dehydrogenase is expressed at high levels in liver, brain, pancreas and kidney, but not in muscle. In the pancreatic cells, GLUD1 is thought to be involved in insulin secretion mechanisms. In nervous tissue, where glutamate is present in concentrations higher than in the other tissues, GLUD1 appears to function in both the synthesis and the catabolism of glutamate and perhaps in ammonia detoxification.

Meglitinides or glinides are a class of drugs used to treat type 2 diabetes.
An ATP-sensitive potassium channel is a type of potassium channel that is gated by intracellular nucleotides, ATP and ADP. ATP-sensitive potassium channels are composed of Kir6.x-type subunits and sulfonylurea receptor (SUR) subunits, along with additional components. KATP channels are widely distributed in plasma membranes; however some may also be found on subcellular membranes. These latter classes of KATP channels can be classified as being either sarcolemmal ("sarcKATP"), mitochondrial ("mitoKATP"), or nuclear ("nucKATP").

Kir6.2 is a major subunit of the ATP-sensitive K+ channel, a lipid-gated inward-rectifier potassium ion channel. The gene encoding the channel is called KCNJ11 and mutations in this gene are associated with congenital hyperinsulinism.

ATP-binding cassette transporter sub-family C member 8 is a protein that in humans is encoded by the ABCC8 gene. ABCC8 orthologs have been identified in all mammals for which complete genome data are available.

G protein-activated inward rectifier potassium channel 2 is a protein that in humans is encoded by the KCNJ6 gene. Mutation in KCNJ6 gene has been proposed to be the cause of Keppen-Lubinsky Syndrome (KPLBS).

Potassium inwardly-rectifying channel, subfamily J, member 8, also known as KCNJ8, is a human gene encoding the Kir6.1 protein. A mutation in KCNJ8 has been associated with cardiac arrest in the early repolarization syndrome.

G protein-activated inward rectifier potassium channel 4(GIRK-4) is a protein that in humans is encoded by the KCNJ5 gene and is a type of G protein-gated ion channel.

Alpha-endosulfine is a protein that in humans is encoded by the ENSA gene.

ATP-binding cassette, sub-family C member 9 (ABCC9) also known as sulfonylurea receptor 2 (SUR2) is an ATP-binding cassette transporter that in humans is encoded by the ABCC9 gene.
The insulin transduction pathway is a biochemical pathway by which insulin increases the uptake of glucose into fat and muscle cells and reduces the synthesis of glucose in the liver and hence is involved in maintaining glucose homeostasis. This pathway is also influenced by fed versus fasting states, stress levels, and a variety of other hormones.
HMR 1883 and its sodium salt HMR 1098, are experimental anti-arrhythmic drugs classified as sulfonylthiourea compounds. Their main purpose is to treat ventricular fibrillation caused by myocardial ischemia. They were synthesized via structural modifications to glibenclamide, an antidiabetic drug. Both HMR 1883 and glibenclamide act by inactivating the ATP-sensitive potassium channels (KATP) responsible for potassium efflux. Unlike glibenclamide, HMR 1883 has been suggested to target selectively the Kir6.2/SUR2A KATP subtype, found mostly in the membranes of cardiac cells. However, data showing that HMR 1098 inhibits the Kir6.2/SUR1 KATP subtype found in insulin-secreting pancreatic beta cells challenges this view.

Colin G. Nichols FRS is the Carl Cori Endowed Professor, and Director of the Center for Investigation of Membrane Excitability Diseases at Washington University in St. Louis, Missouri.
References
- ↑ Campbell JD, Sansom MS, Ashcroft FM (November 2003). "Potassium channel regulation". EMBO Reports. 4 (11): 1038–42. doi:10.1038/sj.embor.embor7400003. PMC 1326373 . PMID 14593442.
- ↑ sulfonylurea+receptor at the U.S. National Library of Medicine Medical Subject Headings (MeSH)
- ↑ Aguilar-Bryan L, Clement JP, Gonzalez G, Kunjilwar K, Babenko A, Bryan J (January 1998). "Toward understanding the assembly and structure of KATP channels". Physiological Reviews. 78 (1): 227–45. doi:10.1152/physrev.1998.78.1.227. PMID 9457174. S2CID 11851627.
- ↑ Nichols CG (March 2006). "KATP channels as molecular sensors of cellular metabolism". Nature. 440 (7083): 470–6. Bibcode:2006Natur.440..470N. doi:10.1038/nature04711. PMID 16554807. S2CID 11899176.
- 1 2 Simard JM, Woo SK, Schwartzbauer GT, Gerzanich V (September 2012). "Sulfonylurea receptor 1 in central nervous system injury: a focused review". Journal of Cerebral Blood Flow and Metabolism. 32 (9): 1699–717. doi:10.1038/jcbfm.2012.91. PMC 3434627 . PMID 22714048.
- 1 2 3 Ortega FJ, Gimeno-Bayon J, Espinosa-Parrilla JF, Carrasco JL, Batlle M, Pugliese M, Mahy N, Rodríguez MJ (May 2012). "ATP-dependent potassium channel blockade strengthens microglial neuroprotection after hypoxia-ischemia in rats". Experimental Neurology. 235 (1): 282–96. doi:10.1016/j.expneurol.2012.02.010. hdl: 2445/34278 . PMID 22387180. S2CID 4828181.
- ↑ Simard JM, Chen M, Tarasov KV, Bhatta S, Ivanova S, Melnitchenko L, Tsymbalyuk N, West GA, Gerzanich V (April 2006). "Newly expressed SUR1-regulated NC(Ca-ATP) channel mediates cerebral edema after ischemic stroke". Nature Medicine. 12 (4): 433–40. doi:10.1038/nm1390. PMC 2740734 . PMID 16550187.
- ↑ Fournet JC, Junien C (2004). "Genetics of congenital hyperinsulinism". Endocrine Pathology. 15 (3): 233–40. doi:10.1385/EP:15:3:233. PMID 15640549. S2CID 24997856.
- ↑ Reis AF, Velho G (February 2002). "Sulfonylurea receptor -1 (SUR1): genetic and metabolic evidences for a role in the susceptibility to type 2 diabetes mellitus". Diabetes & Metabolism. 28 (1): 14–9. PMID 11938023.