Beta cells (β-cells) are a type of cell found in pancreatic islets that synthesize and secrete insulin and amylin. Beta cells make up 50–70% of the cells in human islets. In patients with Type 1 diabetes, beta-cell mass and function are diminished, leading to insufficient insulin secretion and hyperglycemia.
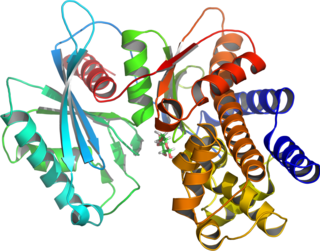
Glucokinase is an enzyme that facilitates phosphorylation of glucose to glucose-6-phosphate. Glucokinase occurs in cells in the liver and pancreas of humans and most other vertebrates. In each of these organs it plays an important role in the regulation of carbohydrate metabolism by acting as a glucose sensor, triggering shifts in metabolism or cell function in response to rising or falling levels of glucose, such as occur after a meal or when fasting. Mutations of the gene for this enzyme can cause unusual forms of diabetes or hypoglycemia.
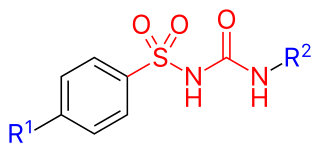
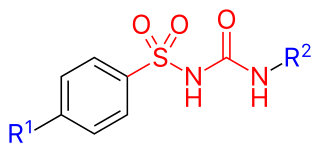
Sulfonylureas or sulphonylureas are a class of organic compounds used in medicine and agriculture. The functional group consists of a sulfonyl group (-S(=O)2) with its sulphur atom bonded to nitrogen atom of a ureylene group (N,N-dehydrourea, a urea derivative). The side chains R1 and R2 distinguish various sulfonylureas.
Maturity-onset diabetes of the young (MODY) refers to any of several hereditary forms of diabetes mellitus caused by mutations in an autosomal dominant gene disrupting insulin production. Along with neonatal diabetes, MODY is a form of the conditions known as monogenic diabetes. While the more common types of diabetes involve more complex combinations of causes involving multiple genes and environmental factors, each forms of MODY are caused by changes to a single gene (monogenic). GCK-MODY and HNF1A-MODY are the most common forms.
Hyperinsulinemic hypoglycemia describes the condition and effects of low blood glucose caused by excessive insulin. Hypoglycemia due to excess insulin is the most common type of serious hypoglycemia. It can be due to endogenous or injected insulin.
Hyperinsulinism refers to an above normal level of insulin in the blood of a person or animal. Normal insulin secretion and blood levels are closely related to the level of glucose in the blood, so that a given level of insulin can be normal for one blood glucose level but low or high for another. Hyperinsulinism can be associated with several types of medical problems, which can be roughly divided into two broad and largely non-overlapping categories: those tending toward reduced sensitivity to insulin and high blood glucose levels (hyperglycemia), and those tending toward excessive insulin secretion and low glucose levels (hypoglycemia).
Nesidioblastosis is a controversial medical term for hyperinsulinemic hypoglycemia attributed to excessive insulin production by pancreatic beta cells that have an abnormal microscopic appearance. The term was coined in the first half of the 20th century. The abnormal microscopic features of the tissue included the presence of islet cell enlargement, pancreatic islet cell dysplasia, beta cells budding from ductal epithelium, and islets in close proximity to ducts.

Congenital hyperinsulinism is a medical term referring to a variety of congenital disorders in which hypoglycemia is caused by excessive insulin secretion. Congenital forms of hyperinsulinemic hypoglycemia can be transient or persistent, mild or severe. These conditions are present at birth and most become apparent in early infancy. Mild cases can be treated by frequent feedings, more severe cases can be controlled by medications that reduce insulin secretion or effects.

Diazoxide, sold under the brand name Proglycem and others, is a medication used to treat low blood sugar due to a number of specific causes. This includes islet cell tumors that cannot be removed and leucine sensitivity. It can also be used in refractory cases of sulfonylurea toxicity. It is generally taken by mouth.

Type 1 diabetes (T1D), formerly known as juvenile diabetes, is an autoimmune disease that originates when cells that make insulin are destroyed by the immune system. Insulin is a hormone required for the cells to use blood sugar for energy and it helps regulate glucose levels in the bloodstream. Before treatment this results in high blood sugar levels in the body. The common symptoms of this elevated blood sugar are frequent urination, increased thirst, increased hunger, weight loss, and other serious complications. Additional symptoms may include blurry vision, tiredness, and slow wound healing. Symptoms typically develop over a short period of time, often a matter of weeks.

GLUD1 is a mitochondrial matrix enzyme, one of the family of glutamate dehydrogenases that are ubiquitous in life, with a key role in nitrogen and glutamate (Glu) metabolism and energy homeostasis. This dehydrogenase is expressed at high levels in liver, brain, pancreas and kidney, but not in muscle. In the pancreatic cells, GLUD1 is thought to be involved in insulin secretion mechanisms. In nervous tissue, where glutamate is present in concentrations higher than in the other tissues, GLUD1 appears to function in both the synthesis and the catabolism of glutamate and perhaps in ammonia detoxification.

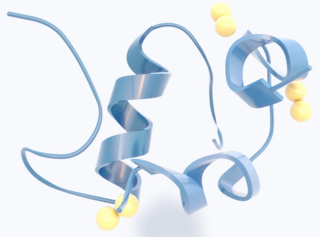
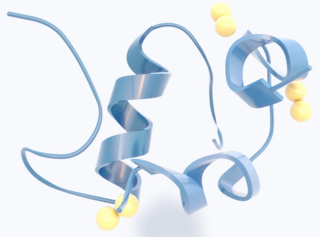
The glucagon-like peptide-1 receptor (GLP1R) is a receptor protein found on beta cells of the pancreas and on neurons of the brain. It is involved in the control of blood sugar level by enhancing insulin secretion. In humans it is synthesised by the gene GLP1R, which is present on chromosome 6. It is a member of the glucagon receptor family of G protein-coupled receptors. GLP1R is composed of two domains, one extracellular (ECD) that binds the C-terminal helix of GLP-1, and one transmembrane (TMD) domain that binds the N-terminal region of GLP-1. In the TMD domain there is a fulcrum of polar residues that regulates the biased signaling of the receptor while the transmembrane helical boundaries and extracellular surface are a trigger for biased agonism.
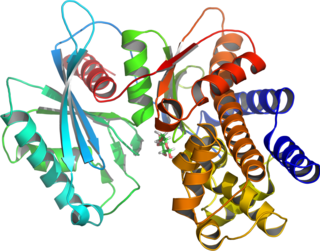
In molecular biology, the sulfonylurea receptors (SUR) are membrane proteins which are the molecular targets of the sulfonylurea class of antidiabetic drugs whose mechanism of action is to promote insulin release from pancreatic beta cells. More specifically, SUR proteins are subunits of the inward-rectifier potassium ion channels Kir6.x. The association of four Kir6.x and four SUR subunits form an ion conducting channel commonly referred to as the KATP channel.

Kir6.2 is a major subunit of the ATP-sensitive K+ channel, a lipid-gated inward-rectifier potassium ion channel. The gene encoding the channel is called KCNJ11 and mutations in this gene are associated with congenital hyperinsulinism.

Alpha-endosulfine is a protein that in humans is encoded by the ENSA gene.

ATP-binding cassette, sub-family C member 9 (ABCC9) also known as sulfonylurea receptor 2 (SUR2) is an ATP-binding cassette transporter that in humans is encoded by the ABCC9 gene.

Hydroxyacyl-Coenzyme A dehydrogenase (HADH) is an enzyme which in humans is encoded by the HADH gene.
MODY 3 or HNF1A-MODY is a form of maturity-onset diabetes of the young. It is caused by mutations of the HNF1-alpha gene, a homeobox gene on human chromosome 12. This is the most common type of MODY in populations with European ancestry, accounting for about 70% of all cases in Europe. HNF1α is a transcription factor that is thought to control a regulatory network important for differentiation of beta cells. Mutations of this gene lead to reduced beta cell mass or impaired function. MODY 1 and MODY 3 diabetes are clinically similar. About 70% of people develop this type of diabetes by age 25 years, but it occurs at much later ages in a few. This type of diabetes can often be treated with sulfonylureas with excellent results for decades. However, the loss of insulin secretory capacity is slowly progressive and most eventually need insulin.

Colin G. Nichols FRS is the Carl Cori Endowed Professor, and Director of the Center for Investigation of Membrane Excitability Diseases at Washington University in St. Louis, Missouri.