Cartilage is a resilient and smooth type of connective tissue. It is a semi-transparent and non-porous type of tissue. It is usually covered by a tough and fibrous membrane called perichondrium. In tetrapods, it covers and protects the ends of long bones at the joints as articular cartilage, and is a structural component of many body parts including the rib cage, the neck and the bronchial tubes, and the intervertebral discs. In other taxa, such as chondrichthyans, but also in cyclostomes, it may constitute a much greater proportion of the skeleton. It is not as hard and rigid as bone, but it is much stiffer and much less flexible than muscle. The matrix of cartilage is made up of glycosaminoglycans, proteoglycans, collagen fibers and, sometimes, elastin. It usually grows quicker than bone.

In humans and other primates, the knee joins the thigh with the leg and consists of two joints: one between the femur and tibia, and one between the femur and patella. It is the largest joint in the human body. The knee is a modified hinge joint, which permits flexion and extension as well as slight internal and external rotation. The knee is vulnerable to injury and to the development of osteoarthritis.
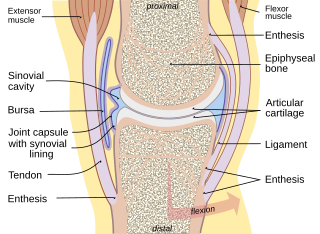
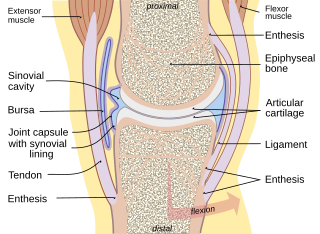
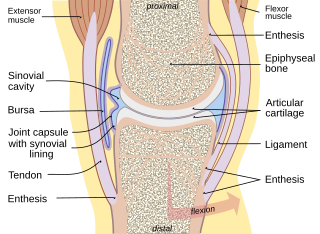
A joint or articulation is the connection made between bones, ossicles, or other hard structures in the body which link an animal's skeletal system into a functional whole. They are constructed to allow for different degrees and types of movement. Some joints, such as the knee, elbow, and shoulder, are self-lubricating, almost frictionless, and are able to withstand compression and maintain heavy loads while still executing smooth and precise movements. Other joints such as sutures between the bones of the skull permit very little movement in order to protect the brain and the sense organs. The connection between a tooth and the jawbone is also called a joint, and is described as a fibrous joint known as a gomphosis. Joints are classified both structurally and functionally.
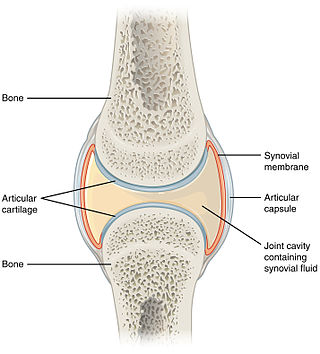
The synovial membrane is a specialized connective tissue that lines the inner surface of capsules of synovial joints, tendon sheaths, and synovial bursas. It makes direct contact with the fibrous membrane on the outside surface and with the synovial fluid lubricant on the inside surface. In contact with the synovial fluid at the tissue surface are many rounded macrophage-like synovial cells and also type B cells, which are also known as fibroblast-like synoviocytes (FLS). Type A cells maintain the synovial fluid by removing wear-and-tear debris. As for the FLS, they produce hyaluronan, as well as other extracellular components in the synovial fluid.

Osteoarthritis (OA) is a type of degenerative joint disease that results from breakdown of joint cartilage and underlying bone. It is believed to be the fourth leading cause of disability in the world, affecting 1 in 7 adults in the United States alone. The most common symptoms are joint pain and stiffness. Usually the symptoms progress slowly over years. Other symptoms may include joint swelling, decreased range of motion, and, when the back is affected, weakness or numbness of the arms and legs. The most commonly involved joints are the two near the ends of the fingers and the joint at the base of the thumbs, the knee and hip joints, and the joints of the neck and lower back. The symptoms can interfere with work and normal daily activities. Unlike some other types of arthritis, only the joints, not internal organs, are affected.
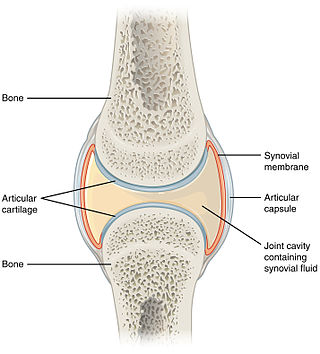
A synovial joint, also known as diarthrosis, joins bones or cartilage with a fibrous joint capsule that is continuous with the periosteum of the joined bones, constitutes the outer boundary of a synovial cavity, and surrounds the bones' articulating surfaces. This joint unites long bones and permits free bone movement and greater mobility. The synovial cavity/joint is filled with synovial fluid. The joint capsule is made up of an outer layer of fibrous membrane, which keeps the bones together structurally, and an inner layer, the synovial membrane, which seals in the synovial fluid.
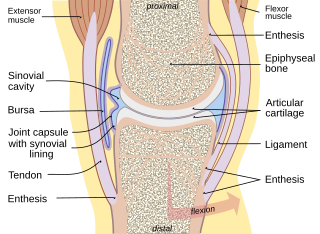
Synovial fluid, also called synovia,[help 1] is a viscous, non-Newtonian fluid found in the cavities of synovial joints. With its egg white–like consistency, the principal role of synovial fluid is to reduce friction between the articular cartilage of synovial joints during movement. Synovial fluid is a small component of the transcellular fluid component of extracellular fluid.

Hyaline cartilage is the glass-like (hyaline) and translucent cartilage found on many joint surfaces. It is also most commonly found in the ribs, nose, larynx, and trachea. Hyaline cartilage is pearl-gray in color, with a firm consistency and has a considerable amount of collagen. It contains no nerves or blood vessels, and its structure is relatively simple.

Enchondroma is a type of benign bone tumor belonging to the group of cartilage tumors. There may be no symptoms, or it may present typically in the short tubular bones of the hands with a swelling, pain or pathological fracture.
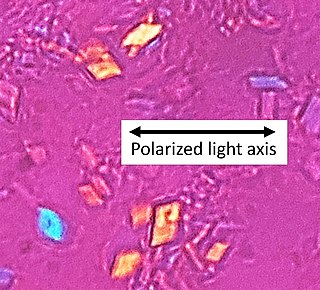
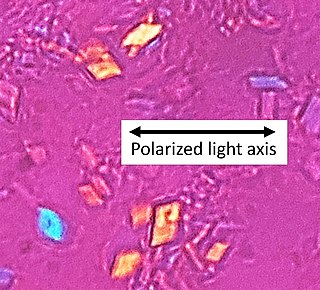
Calcium pyrophosphate dihydrate (CPPD) crystal deposition disease, also known as pseudogout and pyrophosphate arthropathy, is a rheumatologic disease which is thought to be secondary to abnormal accumulation of calcium pyrophosphate dihydrate crystals within joint soft tissues. The knee joint is most commonly affected. The disease is metabolic in origin and its treatment remains symptomatic.

Synovial chondromatosis is a locally aggressive bone tumor of the cartilaginous type. It consists of several hyaline cartilaginous nodules and has the potential of becoming cancerous.

Chondroblastoma is a rare, benign, locally aggressive bone tumor that typically affects the epiphyses or apophyses of long bones. It is thought to arise from an outgrowth of immature cartilage cells (chondroblasts) from secondary ossification centers, originating from the epiphyseal plate or some remnant of it.
Synovectomy is a procedure where the synovial tissue surrounding a joint is removed. This procedure is typically recommended to provide relief from a condition in which the synovial membrane or the joint lining becomes inflamed and irritated and is not controlled by medication alone. If arthritis is not controlled, it can lead to irreversible joint damage. The synovial membrane or "synovium" encloses each joint and also secretes a lubricating fluid that allows different joint motions such as rolling, folding and stretching. When the synovium becomes inflamed or irritated, it increases fluid production, resulting in warmth, tenderness, and swelling in and around the joint.

Proteoglycan 4 or lubricin is a proteoglycan that in humans is encoded by the PRG4 gene. It acts as a joint/boundary lubricant.
Articular cartilage repair treatment involves the repair of the surface of the articular joint's hyaline cartilage, though these solutions do not perfectly restore the articular cartilage. These treatments have been shown to have positive results for patients who have articular cartilage damage. They can provide some measure of pain relief, while slowing down the accumulation of damage, or delaying the need for joint replacement surgery.
Mesenchymal stem cells (MSCs) are multipotent cells found in multiple human adult tissues, including bone marrow, synovial tissues, and adipose tissues. Since they are derived from the mesoderm, they have been shown to differentiate into bone, cartilage, muscle, and adipose tissue. MSCs from embryonic sources have shown promise scientifically while creating significant controversy. As a result, many researchers have focused on adult stem cells, or stem cells isolated from adult humans that can be transplanted into damaged tissue.
Gene therapy for osteoarthritis is the application of gene therapy to treat osteoarthritis (OA). Unlike pharmacological treatments which are administered locally or systemically as a series of interventions, gene therapy aims to establish sustained therapeutic effect after a single, local injection.
The treatment of equine lameness is a complex subject. Lameness in horses has a variety of causes, and treatment must be tailored to the type and degree of injury, as well as the financial capabilities of the owner. Treatment may be applied locally, systemically, or intralesionally, and the strategy for treatment may change as healing progresses. The end goal is to reduce the pain and inflammation associated with injury, to encourage the injured tissue to heal with normal structure and function, and to ultimately return the horse to the highest level of performance possible following recovery.

Pain in the hip is the experience of pain in the muscles or joints in the hip/ pelvic region, a condition commonly arising from any of a number of factors. Sometimes it is closely associated with lower back pain.
A disease-modifying osteoarthritis drug (DMOAD) is a disease-modifying drug that would inhibit or even reverse the progression of osteoarthritis. Since the main hallmark of osteoarthritis is cartilage loss, a typical DMOAD would prevent the loss of cartilage and potentially regenerate it. Other DMOADs may attempt to help repair adjacent tissues by reducing inflammation. A successful DMOAD would be expected to show an improvement in patient pain and function with an improvement of the health of the joint tissues.