In humans and other primates, the knee joins the thigh with the leg and consists of two joints: one between the femur and tibia, and one between the femur and patella. It is the largest joint in the human body. The knee is a modified hinge joint, which permits flexion and extension as well as slight internal and external rotation. The knee is vulnerable to injury and to the development of osteoarthritis.
Tendinopathy is a type of tendon disorder that results in pain, swelling, and impaired function. The pain is typically worse with movement. It most commonly occurs around the shoulder, elbow, wrist, hip, knee, or ankle.

The patella, also known as the kneecap, is a flat, rounded triangular bone which articulates with the femur and covers and protects the anterior articular surface of the knee joint. The patella is found in many tetrapods, such as mice, cats, birds and dogs, but not in whales, or most reptiles.
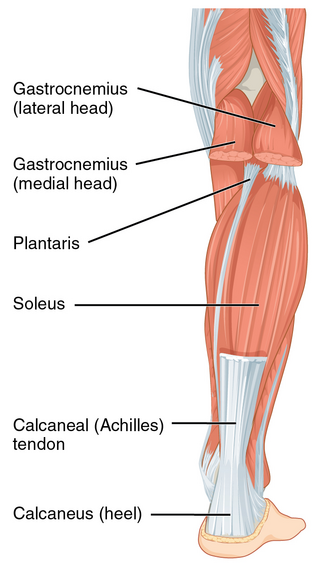
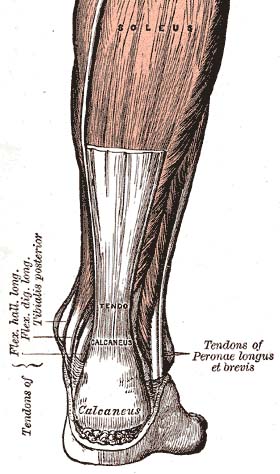
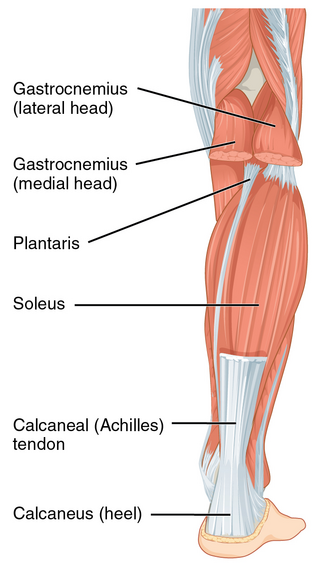
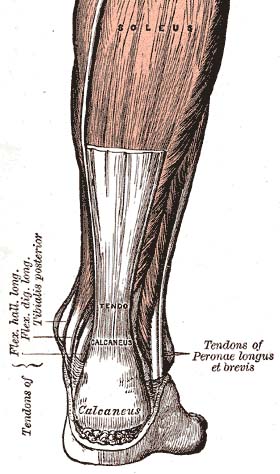
The Achilles tendon or heel cord, also known as the calcaneal tendon, is a tendon at the back of the lower leg, and is the thickest in the human body. It serves to attach the plantaris, gastrocnemius (calf) and soleus muscles to the calcaneus (heel) bone. These muscles, acting via the tendon, cause plantar flexion of the foot at the ankle joint, and flexion at the knee.

A luxating patella, sometimes called a trick knee, is a condition in which the patella, or kneecap, dislocates or moves out of its normal location. It can be associated with damage to the anterior cruciate ligament.

Achilles tendinitis, also known as Achilles tendinopathy, is soreness the Achilles tendon. It is accompanied by alterations in the tendon's structure and mechanical properties. The most common symptoms are pain and swelling around the back of the ankle. The pain is typically worse at the start of exercise and decreases thereafter. Stiffness of the ankle may also be present. Onset is generally gradual.

Osgood–Schlatter disease (OSD) is inflammation of the patellar ligament at the tibial tuberosity (apophysitis) usually affecting adolescents during growth spurts. It is characterized by a painful bump just below the knee that is worse with activity and better with rest. Episodes of pain typically last a few weeks to months. One or both knees may be affected and flares may recur.

Chondromalacia patellae is an inflammation of the underside of the patella and softening of the cartilage.
A negative repetition is the repetition of a technique in weight lifting in which the lifter performs the eccentric phase of a lift. Instead of pressing the weight up slowly, in proper form, a spotter generally aids in the concentric, or lifting, portion of the repetition while the lifter slowly performs the eccentric phase for 3–6 seconds.

Patellar tendon rupture is a tear of the tendon that connects the knee cap (patella) to the tibia. Often there is sudden onset of pain and walking is difficult. In a complete rupture, the ability to extend that knee is decreased. A pop may be felt when it occurs.

A patella fracture is a break of the kneecap. Symptoms include pain, swelling, and bruising to the front of the knee. A person may also be unable to walk. Complications may include injury to the tibia, femur, or knee ligaments.

The unhappy triad, also known as a blown knee among other names, is an injury to the anterior cruciate ligament, medial collateral ligament, and meniscus. Analysis during the 1990s indicated that this 'classic' O'Donoghue triad is actually an unusual clinical entity among athletes with knee injuries. Some authors mistakenly believe that in this type of injury, "combined anterior cruciate and medial collateral ligament disruptions that were incurred during athletic endeavors" always present with concomitant medial meniscus injury. However, the 1990 analysis showed that lateral meniscus tears are more common than medial meniscus tears in conjunction with sprains of the ACL.
Arthrofibrosis has been described in most joints like knee, hip, ankle, foot joints, shoulder, elbow, wrist, hand joints as well as spinal vertebrae. It can occur after injury or surgery or may arise without an obvious cause. There is excessive scar tissue formation within the joint and/or surrounding soft tissues leading to painful restriction of joint motion that persists despite physical therapy and rehabilitation. The scar tissue may be located inside the knee joint or may involve the soft tissue structures around the knee joint, or both locations.

In human anatomy, the quadriceps tendon works with the quadriceps muscle to extend the leg. All four parts of the quadriceps muscle attach to the shin via the patella, where the quadriceps tendon becomes the patellar ligament. It attaches the quadriceps to the top of the patella, which in turn is connected to the shin from its bottom by the patellar ligament. A tendon connects muscle to bone, while a ligament connects bone to bone.

Patellofemoral pain syndrome is knee pain as a result of problems between the kneecap and the femur. The pain is generally in the front of the knee and comes on gradually. Pain may worsen with sitting down with a bent knee for long periods of time, excessive use, or climbing and descending stairs.

A patellar dislocation is a knee injury in which the patella (kneecap) slips out of its normal position. Often the knee is partly bent, painful and swollen. The patella is also often felt and seen out of place. Complications may include a patella fracture or arthritis.

Knee pain is pain in or around the knee.

A quadriceps tendon rupture is a tear of the tendon that runs from the quadriceps muscle to the top of the knee cap.

Volleyball is a game played between two opposing sides, with six players on each team, where the players use mainly their hands to hit the ball over a net and try to make the ball land on the opposing team's side of the court. Volleyball is played by over 800 million people worldwide, making it one of the most popular sports in the world. Volleyball has some risks involved with it because there are some injuries which occur to players that are quite common; these include ankle injuries, shoulder injuries, foot injuries and knee injuries.
Muscle strain is one of the most common injuries in tennis. When an isolated large-energy appears during the muscle contraction and at the same time, bodyweight applies huge amounts of pressure to the lengthened muscle, which can result in the occurrence of muscle strain. Inflammation and bleeding are triggered when muscle strain occur which resulted in redness, pain and swelling. Overuse is also common in tennis players from all levels. Muscle, cartilage, nerves, bursae, ligaments and tendons may be damaged from overuse. The repetitive use of a particular muscle without time for repair and recover in the most common case among the injury.