An arteriovenous malformation (AVM) is an abnormal connection between arteries and veins, bypassing the capillary system. Usually congenital, this vascular anomaly is widely known because of its occurrence in the central nervous system, but can appear anywhere in the body. The symptoms of AVMs can range from none at all to intense pain or bleeding, and they can lead to other serious medical problems.

A cerebral arteriovenous malformation is an abnormal connection between the arteries and veins in the brain—specifically, an arteriovenous malformation in the cerebrum.

Micropsia is a condition affecting human visual perception in which objects are perceived to be smaller than they actually are. Micropsia can be caused by optical factors, by distortion of images in the eye, by changes in the brain, and from psychological factors. Dissociative phenomena are linked with micropsia, which may be the result of brain-lateralization disturbance.
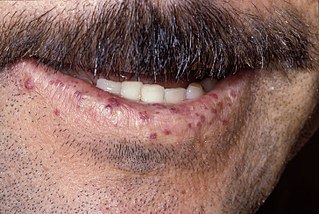
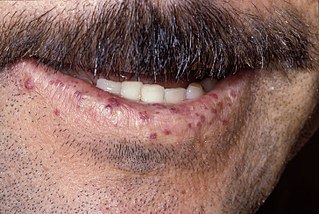
Hereditary hemorrhagic telangiectasia (HHT), also known as Osler–Weber–Rendu disease and Osler–Weber–Rendu syndrome, is a rare autosomal dominant genetic disorder that leads to abnormal blood vessel formation in the skin, mucous membranes, and often in organs such as the lungs, liver, and brain.

Amaurosis fugax is a painless temporary loss of vision in one or both eyes.

Cerebral angiography is a form of angiography which provides images of blood vessels in and around the brain, thereby allowing detection of abnormalities such as arteriovenous malformations and aneurysms. It was pioneered in 1927 by the Portuguese neurologist Egas Moniz at the University of Lisbon, who also helped develop thorotrast for use in the procedure.
Palinopsia is the persistent recurrence of a visual image after the stimulus has been removed. Palinopsia is not a diagnosis; it is a diverse group of pathological visual symptoms with a wide variety of causes. Visual perseveration is synonymous with palinopsia.

Sturge–Weber syndrome, sometimes referred to as encephalotrigeminal angiomatosis, is a rare congenital neurological and skin disorder. It is one of the phakomatoses and is often associated with port-wine stains of the face, glaucoma, seizures, intellectual disability, and ipsilateral leptomeningeal angioma. Sturge–Weber syndrome can be classified into three different types. Type 1 includes facial and leptomeningeal angiomas as well as the possibility of glaucoma or choroidal lesions. Normally, only one side of the brain is affected. This type is the most common. Type 2 involvement includes a facial angioma with a possibility of glaucoma developing. There is no evidence of brain involvement. Symptoms can show at any time beyond the initial diagnosis of the facial angioma. The symptoms can include glaucoma, cerebral blood flow abnormalities and headaches. More research is needed on this type of Sturge–Weber syndrome. Type 3 has leptomeningeal angioma involvement exclusively. The facial angioma is absent and glaucoma rarely occurs. This type is only diagnosed via brain scan.

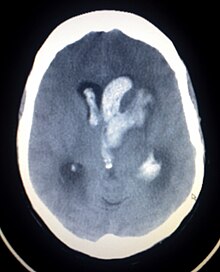
Intraparenchymal hemorrhage (IPH) is one form of intracerebral bleeding in which there is bleeding within brain parenchyma. The other form is intraventricular hemorrhage (IVH).
Optic neuropathy is damage to the optic nerve from any cause. The optic nerve is a bundle of millions of fibers in the retina that sends visual signals to the brain.

Acute posterior multifocal placoid pigment epitheliopathy (APMPPE) is an acquired inflammatory uveitis that belongs to the heterogenous group of white dot syndromes in which light-coloured (yellowish-white) lesions begin to form in the macular area of the retina. Early in the course of the disease, the lesions cause acute and marked vision loss that ranges from mild to severe but is usually transient in nature. APMPPE is classified as an inflammatory disorder that is usually bilateral and acute in onset but self-limiting. The lesions leave behind some pigmentation, but visual acuity eventually improves even without any treatment.
The Center for Cerebrovascular Research at the University of California, San Francisco is a collective of faculty and staff investigating matters related to cerebral circulation, particularly cerebrovascular disease resulting from narrowing of major blood vessels in the brain and vascular malformation of the brain. While research offices are located on Parnassus campus, San Francisco General Hospital hosts the center's laboratories and facilities. The center coordinates with additional faculty in various fields of neuroscience and vascular biology. Sponsors include the National Institute of Neurological Disorders and Stroke and the UCSF departments of Anesthesia, Neurological Surgery and Neurology.
The International Classification of Headache Disorders (ICHD) is a detailed hierarchical classification of all headache-related disorders published by the International Headache Society. It is considered the official classification of headaches by the World Health Organization, and, in 1992, was incorporated into the 10th edition of their International Classification of Diseases (ICD-10). Each class of headache contains explicit diagnostic criteria—meaning that the criteria include quantities rather than vague terms like several or usually—that are based on clinical and laboratory observations.
Cobb syndrome is a rare congenital disorder characterized by visible skin lesions and spinal angiomas or arteriovenous malformations (AVMs). The skin lesions of Cobb syndrome typically are present as port wine stains or angiomas, but reports exist of angiokeratomas, angiolipomas, and lymphangioma circumscriptum. The intraspinal lesions may be angiomas or AVMs and occur at levels of the spinal cord corresponding to the affected skin dermatomes. They may in turn produce spinal cord dysfunction and weakness or paralysis.

Persistent fetal vasculature(PFV), also known as persistent fetal vasculature syndrome (PFVS), and until 1997 known primarily as persistent hyperplastic primary vitreous (PHPV), is a rare congenital anomaly which occurs when blood vessels within the developing eye, known as the embryonic hyaloid vasculature network, fail to regress as they normally would in-utero after the eye is fully developed. Defects which arise from this lack of vascular regression are diverse; as a result, the presentation, symptoms, and prognosis of affected patients vary widely, ranging from clinical insignificance to irreversible blindness. The underlying structural causes of PFV are considered to be relatively common, and the vast majority of cases do not warrant additional intervention. When symptoms do manifest, however, they are often significant, causing detrimental and irreversible visual impairment. Persistent fetal vasculature heightens the lifelong risk of glaucoma, cataracts, intraocular hemorrhages, and Retinal detachments, accounting for the visual loss of nearly 5% of the blind community in the developed world. In diagnosed cases of PFV, approximately 90% of patients with a unilateral disease have associated poor vision in the affected eye.

Parkes Weber syndrome (PWS) is a congenital disorder of the vascular system. It is an extremely rare condition, and its exact prevalence is unknown. It is named after British dermatologist Frederick Parkes Weber, who first described the syndrome in 1907.

Vein of Galen aneurysmal malformations(VGAMs) and Vein of Galen aneurysmal dilations (VGADs) are the most frequent arteriovenous malformations in infants and fetuses. A VGAM consists of a tangled mass of dilated vessels supplied by an enlarged artery. The malformation increases greatly in size with age, although the mechanism of the increase is unknown. Dilation of the great cerebral vein of Galen is a secondary result of the force of arterial blood either directly from an artery via an arteriovenous fistula or by way of a tributary vein that receives the blood directly from an artery. There is usually a venous anomaly downstream from the draining vein that, together with the high blood flow into the great cerebral vein of Galen causes its dilation. The right sided cardiac chambers and pulmonary arteries also develop mild to severe dilation.
Hallucinatory palinopsia is a subtype of palinopsia, a visual disturbance defined as the persistent or recurrence of a visual image after the stimulus has been removed. Palinopsia is a broad term describing a group of symptoms which is divided into hallucinatory palinopsia and illusory palinopsia. Hallucinatory palinopsia refers to the projection of an already-encoded visual memory and is similar to a complex visual hallucination: the creation of a formed visual image where none exists.

CLOVES syndrome is a rare overgrowth syndrome with complex vascular anomalies. CLOVES syndrome affects people with various symptoms, ranging from mild fatty soft-tissue tumors to vascular malformations encompassing the spine or internal organs.

The visual pathway consists of structures that carry visual information from the retina to the brain. Lesions in that pathway cause a variety of visual field defects. In the visual system of human eye, the visual information processed by retinal photoreceptor cells travel in the following way:
Retina→Optic nerve→Optic chiasma →Optic tract→Lateral geniculate body→Optic radiation→Primary visual cortex