Related Research Articles
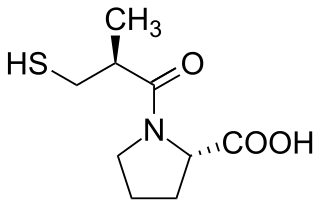
Angiotensin-converting-enzyme inhibitors are a class of medication used primarily for the treatment of high blood pressure and heart failure. This class of medicine works by causing relaxation of blood vessels as well as a decrease in blood volume, which leads to lower blood pressure and decreased oxygen demand from the heart.
Hyponatremia or hyponatraemia is a low concentration of sodium in the blood. It is generally defined as a sodium concentration of less than 135 mmol/L (135 mEq/L), with severe hyponatremia being below 120 mEq/L. Symptoms can be absent, mild or severe. Mild symptoms include a decreased ability to think, headaches, nausea, and poor balance. Severe symptoms include confusion, seizures, and coma; death can ensue.

Ascites is the abnormal build-up of fluid in the abdomen. Technically, it is more than 25 ml of fluid in the peritoneal cavity, although volumes greater than one liter may occur. Symptoms may include increased abdominal size, increased weight, abdominal discomfort, and shortness of breath. Complications can include spontaneous bacterial peritonitis.

Heart failure (HF), also known as congestive heart failure (CHF), is a syndrome caused by an impairment in the heart's ability to fill with and pump blood. Although symptoms vary based on which side of the heart is affected, HF typically presents with shortness of breath, excessive fatigue, and bilateral leg swelling. The severity of the heart failure is mainly decided based on ejection fraction and also measured by the severity of symptoms. Other conditions that have symptoms similar to heart failure include obesity, kidney failure, liver disease, anemia, and thyroid disease.

Furosemide is a loop diuretic medication used to treat edema due to heart failure, liver scarring, or kidney disease. It has had many trade names including Discoid, Frusemide, Lasix and Uremide. Furosemide may also be used for the treatment of high blood pressure. It can be taken intravenously or orally. When given intravenously, furosemide typically takes effect within five minutes; when taken orally, it typically metabolizes within an hour.

Electrolyte imbalance, or water-electrolyte imbalance, is an abnormality in the concentration of electrolytes in the body. Electrolytes play a vital role in maintaining homeostasis in the body. They help to regulate heart and neurological function, fluid balance, oxygen delivery, acid–base balance and much more. Electrolyte imbalances can develop by consuming too little or too much electrolyte as well as excreting too little or too much electrolyte. Examples of electrolytes include calcium, chloride, magnesium, phosphate, potassium, and sodium.

Loop diuretics are diuretics that act on the Na-K-Cl cotransporter along the thick ascending limb of the loop of Henle in nephrons of the kidneys. They are primarily used in medicine to treat hypertension and edema often due to congestive heart failure or chronic kidney disease. While thiazide diuretics are more effective in patients with normal kidney function, loop diuretics are more effective in patients with impaired kidney function.
The syndrome of inappropriate antidiuretic hormone secretion (SIADH), also known as the syndrome of inappropriate antidiuresis (SIAD), is characterized by a physiologically inappropriate release of antidiuretic hormone (ADH) either from the posterior pituitary gland, or an abnormal non-pituitary source. Unsuppressed ADH causes a physiologically inappropriate increase in solute-free water being reabsorbed by the tubules of the kidney to the venous circulation leading to hypotonic hyponatremia.

Chlortalidone, also known as chlorthalidone, is a thiazide-like diuretic drug used to treat high blood pressure, swelling, diabetes insipidus, and renal tubular acidosis. Because chlortalidone is effective in most patients with high blood pressure, it is considered a preferred initial treatment. It is also used to prevent calcium-based kidney stones. It is taken by mouth. Effects generally begin within three hours and last for up to three days. Long-term treatment with chlortalidone is more effective than hydrochlorothiazide for prevention of heart attack or stroke.

Water intoxication, also known as water poisoning, hyperhydration, overhydration, water toxemia or hyponatremia is a potentially fatal disturbance in brain functions that can result when the normal balance of electrolytes in the body is pushed outside safe limits by excessive water intake.

Conivaptan, sold under the brand name Vaprisol, is a non-peptide inhibitor of the receptor for anti-diuretic hormone, also called vasopressin. It was approved in 2004 for hyponatremia. The compound was discovered by Astellas and marked in 2006. The drug is now marketed by Cumberland Pharmaceuticals, Inc.

Hepatorenal syndrome is a life-threatening medical condition that consists of rapid deterioration in kidney function in individuals with cirrhosis or fulminant liver failure. HRS is usually fatal unless a liver transplant is performed, although various treatments, such as dialysis, can prevent advancement of the condition.
Fluid balance is an aspect of the homeostasis of organisms in which the amount of water in the organism needs to be controlled, via osmoregulation and behavior, such that the concentrations of electrolytes in the various body fluids are kept within healthy ranges. The core principle of fluid balance is that the amount of water lost from the body must equal the amount of water taken in; for example, in humans, the output must equal the input. Euvolemia is the state of normal body fluid volume, including blood volume, interstitial fluid volume, and intracellular fluid volume; hypovolemia and hypervolemia are imbalances. Water is necessary for all life on Earth. Humans can survive for 4 to 6 weeks without food but only for a few days without water.

Hypervolemia, also known as fluid overload, is the medical condition where there is too much fluid in the blood. The opposite condition is hypovolemia, which is too little fluid volume in the blood. Fluid volume excess in the intravascular compartment occurs due to an increase in total body sodium content and a consequent increase in extracellular body water. The mechanism usually stems from compromised regulatory mechanisms for sodium handling as seen in congestive heart failure (CHF), kidney failure, and liver failure. It may also be caused by excessive intake of sodium from foods, intravenous (IV) solutions and blood transfusions, medications, or diagnostic contrast dyes. Treatment typically includes administration of diuretics and limit the intake of water, fluids, sodium, and salt.
Primary polydipsia and psychogenic polydipsia are forms of polydipsia characterised by excessive fluid intake in the absence of physiological stimuli to drink. Psychogenic polydipsia which is caused by psychiatric disorders, often schizophrenia, is often accompanied by the sensation of dry mouth. Some forms of polydipsia are explicitly non-psychogenic. Primary polydipsia is a diagnosis of exclusion.
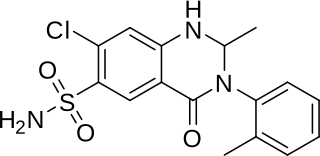
Metolazone is a thiazide-like diuretic marketed under the brand names Zytanix, Metoz, Zaroxolyn, and Mykrox. It is primarily used to treat congestive heart failure and high blood pressure. Metolazone indirectly decreases the amount of water reabsorbed into the bloodstream by the kidney, so that blood volume decreases and urine volume increases. This lowers blood pressure and prevents excess fluid accumulation in heart failure. Metolazone is sometimes used together with loop diuretics such as furosemide or bumetanide, but these highly effective combinations can lead to dehydration and electrolyte abnormalities.
A vasopressin receptor antagonist (VRA) is an agent that interferes with action at the vasopressin receptors. Most commonly VRAs are used in the treatment of hyponatremia, especially in patients with congestive heart failure, liver cirrhosis or SIADH.
Hypoosmolar hyponatremia is a condition where hyponatremia is associated with a low plasma osmolality. The term "hypotonic hyponatremia" is also sometimes used.
Management of heart failure requires a multimodal approach. It involves a combination of lifestyle modifications, medications, and possibly the use of devices or surgery.

A diuretic is any substance that promotes diuresis, the increased production of urine. This includes forced diuresis. A diuretic tablet is sometimes colloquially called a water tablet. There are several categories of diuretics. All diuretics increase the excretion of water from the body, through the kidneys. There exist several classes of diuretic, and each works in a distinct way. Alternatively, an antidiuretic, such as vasopressin, is an agent or drug which reduces the excretion of water in urine.
References
- ↑ "Fluid Restricted Diet". intermountainphysician.org. 2016. Archived from the original on 12 August 2020. Retrieved 16 December 2019.
- ↑ Debra K. Moser; Barbara Riegel (2001). Improving Outcomes in Heart Failure: An Interdisciplinary Approach. Jones & Bartlett Learning. pp. 310–. ISBN 978-0-8342-1644-0.
- ↑ "Fluid Restricted Diet". Winchester Hospital. Retrieved 16 December 2019.
- ↑ NEMO (2017). "Controlling fluid intake in heart failure" (PDF). health.qld.gov.au. Retrieved 16 December 2019.
- ↑ Byock I (1995). "Patient refusal of nutrition and hydration: walking the ever-finer line". Am J Hosp Palliat Care. 12 (2): 8, 9–13. doi:10.1177/104990919501200205. PMID 7605733. S2CID 46385519.
- 1 2 Gheorghiade, Mihai; Gottlieb, Stephen S.; Udelson, James E.; Konstam, Marvin A.; Czerwiec, Frank; Ouyang, John; Orlandi, Cesare (2006). "Vasopressin V2 Receptor Blockade With Tolvaptan Versus Fluid Restriction in the Treatment of Hyponatremia". The American Journal of Cardiology. 97 (7): 1064–1067. doi:10.1016/j.amjcard.2005.10.050. PMID 16563917.
- ↑ Tai MK (2009). "Evidence-based practice of fluid restriction in patients with heart failure". Hu Li Za Zhi (in Chinese). 56 (5): 23–9. PMID 19760574.
- ↑ The CONSENSUS Trial Study Group. (1987). "Effects of enalapril on mortality in severe congestive heart failure. Results of the Cooperative North Scandinavian Enalapril Survival Study (CONSENSUS)". N Engl J Med. 316 (23): 1429–35. doi:10.1056/NEJM198706043162301. PMID 2883575.
- ↑ The SOLVD Investigators. (1991). "Effect of enalapril on survival in patients with reduced left ventricular ejection fractions and congestive heart failure". N Engl J Med. 325 (5): 293–302. doi: 10.1056/NEJM199108013250501 . PMID 2057034.
- ↑ Schürer, Ludwig; Wolf, Stefan; Lumenta, Christianto B. (2010). "Water and Electrolyte Regulation". Neurosurgery. pp. 611–615. doi:10.1007/978-3-540-79565-0_40. ISBN 978-3-540-79564-3.