Related Research Articles

The brachial plexus is a network of nerves formed by the anterior rami of the lower four cervical nerves and first thoracic nerve. This plexus extends from the spinal cord, through the cervicoaxillary canal in the neck, over the first rib, and into the armpit, it supplies afferent and efferent nerve fibers to the chest, shoulder, arm, forearm, and hand.

The phrenic nerve is a mixed motor/sensory nerve that originates from the C3-C5 spinal nerves in the neck. The nerve is important for breathing because it provides exclusive motor control of the diaphragm, the primary muscle of respiration. In humans, the right and left phrenic nerves are primarily supplied by the C4 spinal nerve, but there is also a contribution from the C3 and C5 spinal nerves. From its origin in the neck, the nerve travels downward into the chest to pass between the heart and lungs towards the diaphragm.
Paresthesia is an abnormal sensation of the skin with no apparent physical cause. Paresthesia may be transient or chronic, and may have many possible underlying causes. Paresthesias are usually painless and can occur anywhere on the body, but most commonly occur in the arms and legs.
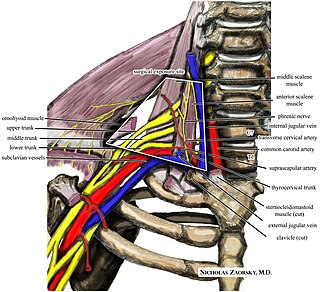
Thoracic outlet syndrome (TOS) is a condition in which there is compression of the nerves, arteries, or veins in the superior thoracic aperture, the passageway from the lower neck to the armpit, also known as the thoracic outlet. There are three main types: neurogenic, venous, and arterial. The neurogenic type is the most common and presents with pain, weakness, paraesthesia, and occasionally loss of muscle at the base of the thumb. The venous type results in swelling, pain, and possibly a bluish coloration of the arm. The arterial type results in pain, coldness, and pallor of the arm.
A side stitch is an intense stabbing abdominal pain under the lower edge of the ribcage that occurs during exercise. It is also called a side ache, side cramp, muscle stitch, or simply stitch, and the medical term is exercise-related transient abdominal pain (ETAP). It sometimes extends to shoulder tip pain, and commonly occurs during running, swimming, and horseback riding. Approximately two-thirds of runners will experience at least one episode of a stitch each year. The precise cause is unclear, although it most likely involves irritation of the abdominal lining, and the condition is more likely after consuming a meal or a sugary beverage. If the pain is present only when exercising and is completely absent at rest, in an otherwise healthy person, it does not require investigation. Typical treatment strategies involve deep breathing and/or manual pressure on the affected area.

The musculocutaneous nerve is a mixed branch of the lateral cord of the brachial plexus derived from cervical spinal nerves C5-C7. It arises opposite the lower border of the pectoralis major. It provides motor innervation to the muscles of the anterior compartment of the arm: the coracobrachialis, biceps brachii, and brachialis. It provides sensory innervation to the lateral forearm. It courses through the anterior part of the arm, terminating 2 cm above elbow; after passing the lateral edge of the tendon of biceps brachii it is becomes known as the lateral cutaneous nerve of the forearm.
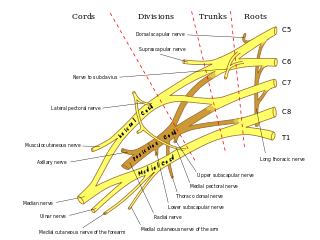
Erb's palsy is a paralysis of the arm caused by injury to the upper group of the arm's main nerves, specifically the severing of the upper trunk C5–C6 nerves. These form part of the brachial plexus, comprising the ventral rami of spinal nerves C5–C8 and thoracic nerve T1. These injuries arise most commonly, but not exclusively, from shoulder dystocia during a difficult birth. Depending on the nature of the damage, the paralysis can either resolve on its own over a period of months, necessitate rehabilitative therapy, or require surgery.

Shoulder dystocia is when, after vaginal delivery of the head, the baby's anterior shoulder gets caught above the mother's pubic bone. Signs include retraction of the baby's head back into the vagina, known as "turtle sign". Complications for the baby may include brachial plexus injury, or clavicle fracture. Complications for the mother may include vaginal or perineal tears, postpartum bleeding, or uterine rupture.

Nerve block or regional nerve blockade is any deliberate interruption of signals traveling along a nerve, often for the purpose of pain relief. Local anesthetic nerve block is a short-term block, usually lasting hours or days, involving the injection of an anesthetic, a corticosteroid, and other agents onto or near a nerve. Neurolytic block, the deliberate temporary degeneration of nerve fibers through the application of chemicals, heat, or freezing, produces a block that may persist for weeks, months, or indefinitely. Neurectomy, the cutting through or removal of a nerve or a section of a nerve, usually produces a permanent block. Because neurectomy of a sensory nerve is often followed, months later, by the emergence of new, more intense pain, sensory nerve neurectomy is rarely performed.

The shoulder joint is structurally classified as a synovial ball-and-socket joint and functionally as a diarthrosis and multiaxial joint. It involves an articulation between the glenoid fossa of the scapula and the head of the humerus. Due to the very loose joint capsule that gives a limited interface of the humerus and scapula, it is the most mobile joint of the human body.

A brachial plexus injury (BPI), also known as brachial plexus lesion, is an injury to the brachial plexus, the network of nerves that conducts signals from the spinal cord to the shoulder, arm and hand. These nerves originate in the fifth, sixth, seventh and eighth cervical (C5–C8), and first thoracic (T1) spinal nerves, and innervate the muscles and skin of the chest, shoulder, arm and hand.
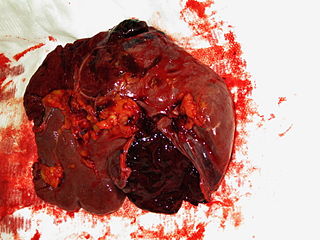
A splenic injury, which includes a ruptured spleen, is any injury to the spleen. The rupture of a normal spleen can be caused by trauma, such as a traffic collision.

A spinal disc herniation is an injury to the intervertebral disc between two spinal vertebrae, usually caused by excessive strain or trauma to the spine. It may result in back pain, pain or sensation in different parts of the body, and physical disability. The most conclusive diagnostic tool for disc herniation is MRI, and treatment may range from painkillers to surgery. Protection from disc herniation is best provided by core strength and an awareness of body mechanics including good posture.

Radiculopathy, also commonly referred to as pinched nerve, refers to a set of conditions in which one or more nerves are affected and do not work properly. Radiculopathy can result in pain, weakness, altered sensation (paresthesia) or difficulty controlling specific muscles. Pinched nerves arise when surrounding bone or tissue, such as cartilage, muscles or tendons, put pressure on the nerve and disrupt its function.
Johannes Otto Kehr was a German surgeon and professor of surgery. Kehr was born in Waltershausen, Saxe-Coburg and Gotha.

Hereditary neuralgic amyotrophy (HNA) is a neuralgic disorder that is characterized by nerve damage and muscle atrophy, preceded by severe pain. In about half of the cases it is associated with a mutation of the SEPT9 gene (17q25). While not much is known about this disorder, it has been characterized to be similar to Parsonage-Turner syndrome in prognosis.

Cervical spinal nerve 4, also called C4, is a spinal nerve of the cervical segment. It originates from the spinal cord above the 4th cervical vertebra (C4). It contributes nerve fibers to the phrenic nerve, the motor nerve to the thoracoabdominal diaphragm. It also provides motor nerves for the longus capitis, longus colli, anterior scalene, middle scalene, and levator scapulae muscles. C4 contributes some sensory fibers to the supraclavicular nerves, responsible for sensation from the skin above the clavicle. C4 and C5 are the areas that see the highest amount of cervical spine trauma.

Nerve compression syndrome, or compression neuropathy, or nerve entrapment syndrome, is a medical condition caused by chronic, direct pressure on a peripheral nerve. It is known colloquially as a trapped nerve, though this may also refer to nerve root compression. Its symptoms include pain, tingling, numbness and muscle weakness. The symptoms affect just one particular part of the body, depending on which nerve is affected. The diagnosis is largely clinical and can be confirmed with diagnostic nerve blocks. Occasionally imaging and electrophysiology studies aid in the diagnosis. Timely diagnosis is important as untreated chronic nerve compression may cause permanent damage. A surgical nerve decompression can relieve pressure on the nerve but cannot always reverse the physiological changes that occurred before treatment. Nerve injury by a single episode of physical trauma is in one sense an acute compression neuropathy but is not usually included under this heading, as chronic compression takes a unique pathophysiological course.

Brachial plexus block is a regional anesthesia technique that is sometimes employed as an alternative or as an adjunct to general anesthesia for surgery of the upper extremity. This technique involves the injection of local anesthetic agents in close proximity to the brachial plexus, temporarily blocking the sensation and ability to move the upper extremity. The subject can remain awake during the ensuing surgical procedure, or they can be sedated or even fully anesthetized if necessary.
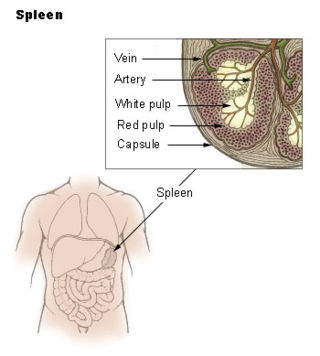
Spleen pain is a pain felt from the left upper quadrant of the abdomen or epigastrium where the human spleen is located or neighboring.
References
- ↑ Rutkow IM (June 1978). "Rupture of the spleen in infectious mononucleosis: a critical review". Arch Surg. 113 (6): 718–20. doi:10.1001/archsurg.1978.01370180060007. PMID 655846.
- ↑ Betts, J Gordon; Desaix, Peter; Johnson, Eddie; Johnson, Jody E; Korol, Oksana; Kruse, Dean; Poe, Brandon; Wise, James; Womble, Mark D; Young, Kelly A (June 8, 2023). Anatomy & Physiology. Houston: OpenStax CNX. 15.2 Autonomic reflexes and homeostasis. ISBN 978-1-947172-04-3.
- ↑ Klimpel V (2004). "Does Kehr's sign derive from Hans Kehr? A critical commentary on its documentation?". Der Chirurg. 75 (1): 80–3. doi:10.1007/s00104-003-0796-2. PMID 14740133. S2CID 22705413.