Related Research Articles

Parkinsonism is a clinical syndrome characterized by tremor, bradykinesia, rigidity, and postural instability. These are the four motor symptoms found in Parkinson's disease (PD) – after which it is named – dementia with Lewy bodies (DLB), Parkinson's disease dementia (PDD), and many other conditions. This set of symptoms occurs in a wide range of conditions and may have many causes, including neurodegenerative conditions, drugs, toxins, metabolic diseases, and neurological conditions other than PD.

Dementia with Lewy bodies (DLB) is a type of dementia characterized by changes in sleep, behavior, cognition, movement, and regulation of automatic bodily functions. Memory loss is not always an early symptom. The disease worsens over time and is usually diagnosed when cognitive impairment interferes with normal daily functioning. Together with Parkinson's disease dementia, DLB is one of the two Lewy body dementias. It is a common form of dementia, but the prevalence is not known accurately and many diagnoses are missed. The disease was first described by Kenji Kosaka in 1976.
Lewy body dementias are two similar and common subtypes of dementia: Dementia with Lewy bodies (DLB) and Parkinson's disease dementia (PDD). Both are characterized by changes in thinking, movement, behavior, and mood. The two conditions have similar features and may have similar causes, and are believed to belong on a spectrum of Lewy body disease that includes Parkinson's disease. As of 2014, they were more often misdiagnosed than any other common dementia.

Rapid eye movement sleep behavior disorder or REM behavior disorder (RBD) is a sleep disorder in which people act out their dreams. It involves abnormal behavior during the sleep phase with rapid eye movement (REM) sleep. The major feature of RBD is loss of muscle atonia during otherwise intact REM sleep. The loss of motor inhibition leads to sleep behaviors ranging from simple limb twitches to more complex integrated movements that can be violent or result in injury to either the individual or their bedmates.

Multiple system atrophy (MSA) is a rare neurodegenerative disorder characterized by autonomic dysfunction, tremors, slow movement, muscle rigidity, and postural instability and ataxia. This is caused by progressive degeneration of neurons in several parts of the brain including the basal ganglia, inferior olivary nucleus, and cerebellum.

Progressive supranuclear palsy (PSP) is a late-onset neurodegenerative disease involving the gradual deterioration and death of specific volumes of the brain. The condition leads to symptoms including loss of balance, slowing of movement, difficulty moving the eyes, and cognitive impairment. PSP may be mistaken for other types of neurodegeneration such as Parkinson's disease, frontotemporal dementia and Alzheimer's disease. The cause of the condition is uncertain, but involves the accumulation of tau protein within the brain. Medications such as levodopa and amantadine may be useful in some cases.

Corticobasal degeneration (CBD) is a rare neurodegenerative disease involving the cerebral cortex and the basal ganglia. CBD symptoms typically begin in people from 50 to 70 years of age, and the average disease duration is six years. It is characterized by marked disorders in movement and cognition, and is classified as one of the Parkinson plus syndromes. Diagnosis is difficult, as symptoms are often similar to those of other disorders, such as Parkinson's disease, progressive supranuclear palsy, and dementia with Lewy bodies, and a definitive diagnosis of CBD can only be made upon neuropathologic examination.

Tauopathy belongs to a class of neurodegenerative diseases involving the aggregation of tau protein into neurofibrillary or gliofibrillary tangles in the human brain. Tangles are formed by hyperphosphorylation of the microtubule protein known as tau, causing the protein to dissociate from microtubules and form insoluble aggregates. The mechanism of tangle formation is not well understood, and whether tangles are a primary cause of Alzheimer's disease or play a peripheral role is unknown.

Frontotemporal dementia and parkinsonism linked to chromosome 17 (FTDP-17) is an autosomal dominant neurodegenerative tauopathy and Parkinson plus syndrome. FTDP-17 is caused by mutations in the MAPT gene located on the q arm of chromosome 17, and has three cardinal features: behavioral and personality changes, cognitive impairment, and motor symptoms. FTDP-17 was defined during the International Consensus Conference in Ann Arbor, Michigan, in 1996.
DaT Scan commonly refers to a diagnostic method, based on SPECT imaging, to investigate if there is a loss of dopaminergic neurons in striatum. The term may also refer to a brand name of Ioflupane (123I) tracer used for the study. The scan principle is based on use of the radiopharmaceutical Ioflupane (123I) which binds to dopamine transporters (DaT). The signal from them is then detected by the use of single-photon emission computed tomography (SPECT) which uses special gamma-cameras to create a pictographic representation of the distribution of dopamine transporters in the brain.

Parkinson's disease (PD), or simply Parkinson's, is a chronic degenerative disorder of the central nervous system that affects both the motor system and non-motor systems. The symptoms usually emerge slowly, and as the disease worsens, non-motor symptoms become more common. Early symptoms are tremor, rigidity, slowness of movement, and difficulty with walking. Problems may also arise with cognition, behaviour, sleep, and sensory systems. Parkinson's disease dementia becomes common in advanced stages of the disease.
The applause sign is a behavioural indicator, relevant to neurodegenerative conditions, characterised by a patient’s inability to execute the same number of hand claps as demonstrated by an examiner.
Signs and symptoms of Parkinson's disease are varied. Parkinson's disease affects movement, producing motor symptoms. Non-motor symptoms, which include dysautonomia, cognitive and neurobehavioral problems, and sensory and sleep difficulties, are also common. When other diseases mimic Parkinson's disease, they are categorized as parkinsonism.

Kufor–Rakeb syndrome (KRS) is an autosomal recessive disorder of juvenile onset also known as Parkinson disease-9 (PARK9). It is named after Kufr Rakeb in Irbid, Jordan. Kufor–Rakeb syndrome was first identified in this region in Jordan with a Jordanian couple's 5 children who had rigidity, mask-like face, and bradykinesia. The disease was first described in 1994 by Najim Al-Din et al. The OMIM number is 606693.

The history of Parkinson's disease expands from 1817, when British apothecary James Parkinson published An Essay on the Shaking Palsy, to modern times. Before Parkinson's descriptions, others had already described features of the disease that would bear his name, while the 20th century greatly improved knowledge of the disease and its treatments. PD was then known as paralysis agitans. The term "Parkinson's disease" was coined in 1865 by William Sanders and later popularized by French neurologist Jean-Martin Charcot. Paralysis
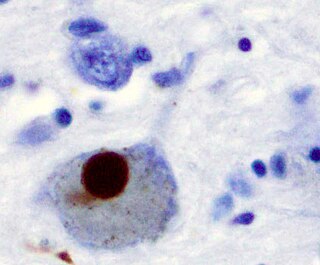
Synucleinopathies are neurodegenerative diseases characterised by the abnormal accumulation of aggregates of alpha-synuclein protein in neurons, nerve fibres or glial cells. There are three main types of synucleinopathy: Parkinson's disease (PD), dementia with Lewy bodies (DLB), and multiple system atrophy (MSA). Other rare disorders, such as various neuroaxonal dystrophies, also have α-synuclein pathologies. Additionally, autopsy studies have shown that around 6% of sporadic Alzheimer's Disease exhibit α-synuclein positive Lewy pathology, and are sub-classed as Alzheimer's Disease with Amygdalar Restricted Lewy Bodies (AD/ALB).
Parkinson's disease dementia (PDD) is dementia that is associated with Parkinson's disease (PD). Together with dementia with Lewy bodies (DLB), it is one of the Lewy body dementias characterized by abnormal deposits of Lewy bodies in the brain.
Corticobasal syndrome (CBS) is a rare, progressive atypical Parkinsonism syndrome and is a tauopathy related to frontotemporal dementia. CBS is typically caused by the deposit of tau proteins forming in different areas of the brain.
The Frontal Assessment Battery (FAB) is a short screening test to evaluate executive function (EF).
Rapid eye movement sleep behaviour disorder and Parkinson's disease is rapid eye movement sleep behavior disorder (RBD) that is associated with Parkinson's disease. RBC is linked genetically and neuropathologically to α- synuclein, a presynaptic neuronal protein that exerts deleterious effects on neighbouring proteins, leading to neuronal death. This pathology is linked to numerous other neurodegenerative disorders, such as Lewy bodies dementia, and collectively these disorders are known as synucleinopathies. Numerous reports over the past few years have stated the frequent association of synucleinopathies with REM sleep behaviour disorder (RBD). In particular, the frequent association of RBD with Parkinson's. In the general population the incidence of RBD is around 0.5%, compared to the prevalence of RBD in PD patients, which has been reported to be between 38% and 60%. The diagnosis and symptom onset of RBD typically precedes the onset of motor or cognitive symptoms of PD by a number of years, typically ranging anywhere from 2 to 15 years prior. Hence, this link could provide an important window of opportunity in the implementation of therapies and treatments, that could prevent or slow the onset of PD.
References
- ↑ Bensimon G, Ludolph A, Agid Y, Vidailhet M, Payan C, Leigh PN (January 2009). "Riluzole treatment, survival and diagnostic criteria in Parkinson plus disorders: the NNIPPS study". Brain. 132 (Pt 1): 156–71. doi:10.1093/brain/awn291. PMC 2638696 . PMID 19029129.
- 1 2 3 4 Mitra K.; Gangopadhaya P. K.; Das S. K. (2003). "Parkinsonism plus syndrome—a review". Neurol India. 51 (2): 183–188. PMID 14570999.
- ↑ Vertes, Alex C.; Beato, Morris R.; Sonne, James; Khan Suheb, Mahammed Z. (2022). "Parkinson-plus Syndrome". StatPearls. StatPearls Publishing. PMID 36256760 . Retrieved 20 February 2023.
- ↑ Mark, M. H. (2001). "Lumping and splitting the Parkinson Plus syndromes: dementia with Lewy bodies, multiple system atrophy, progressive supranuclear palsy, and cortical-basal ganglionic degeneration". Neurologic Clinics. 19 (3): 607–27. doi:10.1016/S0733-8619(05)70037-2. PMID 11532646.
- ↑ Levin J, Kurz A, Arzberger T, Giese A, Höglinger GU (February 5, 2016). "The Differential Diagnosis and Treatment of Atypical Parkinsonism". Dtsch Ärztebl Int. 113 (5): 61–9. doi:10.3238/arztebl.2016.0061. PMC 4782269 . PMID 26900156.
- ↑ Brittany N. Dugger; Charles H. Adler; Holly A. Shill; John Caviness; Sandra Jacobson; Erika Driver-Dunckley; Thomas G. Beach & the Arizona Parkinson’s Disease Consortium (May 2014). "Concomitant pathologies among a spectrum of parkinsonian disorders". Parkinsonism Relat Disord. 20 (5): 525–9. doi:10.1016/j.parkreldis.2014.02.012. PMC 4028418 . PMID 24637124.
- ↑ Constance Ward (2006). "Characteristics and symptom management of progressive supranuclear palsy: a multidisciplinary approach" (PDF). Journal of Neuroscience Nursing. 38 (4): 242–247. doi:10.1097/01376517-200608000-00007. PMID 16925000. Archived from the original (PDF) on 2008-07-23.
- ↑ "Multiple System Atrophy with Orthostatic Hypotension Information Page". Archived from the original on 2012-05-14. Retrieved 2009-09-15.
- ↑ Hierholzer, Johannes; Cordes, Michael; Venz, Stephan; Schelosky, Ludwig; Harisch, Cordula; Richter, Wolf; Keske, Uwe; Hosten, Norbert; Mäurer, Jürgen (1998-06-01). "Loss of Dopamine-D2 Receptor Binding Sites in Parkinsonian Plus Syndromes". Journal of Nuclear Medicine. 39 (6): 954–960. ISSN 0161-5505. PMID 9627325.
- ↑ Litvan I, Campbell G, Mangone CA, Verny M, McKee A, Chaudhuri KR, Jellinger K, Pearce RK, D'Olhaberriague L (Jan 1997). "Which clinical features differentiate progressive supranuclear palsy (Steele-Richardson-Olzewski syndrome) from related disorders". Brain. 120 (1): 65–74. doi: 10.1093/brain/120.1.65 . PMID 9055798.
- ↑ David R. Williams & Irene Litvan (October 2013). "Parkinsonian syndromes". Continuum (Minneap Minn). 19 (5 Movement Disorders): 1189–212. doi:10.1212/01.CON.0000436152.24038.e0. PMC 4234134 . PMID 24092286.
- ↑ Molloy, F. M., & Healy, D. G. (2011). Parkinsonism Plus Syndromes. In O. Hardiman & C. P. Doherty (Eds.), Neurodegenerative Disorders (181-196). London: Springer London. doi : 10.1007/978-1-84996-011-3_9
- ↑ Ling H (2016). "Clinical Approach to Progressive Supranuclear Palsy". J Mov Disord. 9 (1): 3–13. doi:10.14802/jmd.15060. PMC 4734991 . PMID 26828211.