The aorta is the main and largest artery in the human body, originating from the left ventricle of the heart, branching upwards immediately after, and extending down to the abdomen, where it splits at the aortic bifurcation into two smaller arteries. The aorta distributes oxygenated blood to all parts of the body through the systemic circulation.

The pleural cavity, pleural space, or intrapleural space is the potential space between the pleurae of the pleural sac that surrounds each lung. A small amount of serous pleural fluid is maintained in the pleural cavity to enable lubrication between the membranes, and also to create a pressure gradient.

The pericardium, also called pericardial sac, is a double-walled sac containing the heart and the roots of the great vessels. It has two layers, an outer layer made of strong inelastic connective tissue, and an inner layer made of serous membrane. It encloses the pericardial cavity, which contains pericardial fluid, and defines the middle mediastinum. It separates the heart from interference of other structures, protects it against infection and blunt trauma, and lubricates the heart's movements.

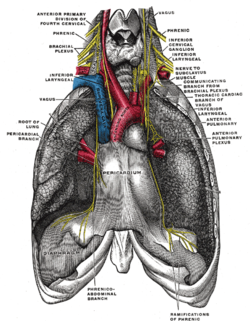
The phrenic nerve is a mixed motor/sensory nerve that originates from the C3-C5 spinal nerves in the neck. The nerve is important for breathing because it provides exclusive motor control of the diaphragm, the primary muscle of respiration. In humans, the right and left phrenic nerves are primarily supplied by the C4 spinal nerve, but there is also a contribution from the C3 and C5 spinal nerves. From its origin in the neck, the nerve travels downward into the chest to pass between the heart and lungs towards the diaphragm.

In human anatomy, the subclavian arteries are paired major arteries of the upper thorax, below the clavicle. They receive blood from the aortic arch. The left subclavian artery supplies blood to the left arm and the right subclavian artery supplies blood to the right arm, with some branches supplying the head and thorax. On the left side of the body, the subclavian comes directly off the aortic arch, while on the right side it arises from the relatively short brachiocephalic artery when it bifurcates into the subclavian and the right common carotid artery.

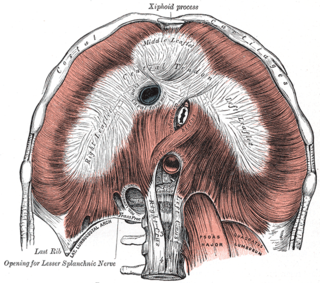
The thoracic diaphragm, or simply the diaphragm, is a sheet of internal skeletal muscle in humans and other mammals that extends across the bottom of the thoracic cavity. The diaphragm is the most important muscle of respiration, and separates the thoracic cavity, containing the heart and lungs, from the abdominal cavity: as the diaphragm contracts, the volume of the thoracic cavity increases, creating a negative pressure there, which draws air into the lungs. Its high oxygen consumption is noted by the many mitochondria and capillaries present; more than in any other skeletal muscle.

The cervical plexus is a nerve plexus of the anterior rami of the first four cervical spinal nerves C1-C4. The cervical plexus provides motor innervation to some muscles of the neck, and the diaphragm; it provides sensory innervation to parts of the head, neck, and chest.

The mediastinum is the central compartment of the thoracic cavity. Surrounded by loose connective tissue, it is an undelineated region that contains a group of structures within the thorax, namely the heart and its vessels, the esophagus, the trachea, the phrenic and cardiac nerves, the thoracic duct, the thymus and the lymph nodes of the central chest.

In human anatomy, the internal thoracic artery (ITA), also known as the internal mammary artery, is an artery that supplies the anterior chest wall and the breasts. It is a paired artery, with one running along each side of the sternum, to continue after its bifurcation as the superior epigastric and musculophrenic arteries.

The thoracic aorta is a part of the aorta located in the thorax. It is a continuation of the aortic arch. It is located within the posterior mediastinal cavity, but frequently bulges into the left pleural cavity. The descending thoracic aorta begins at the lower border of the fourth thoracic vertebra and ends in front of the lower border of the twelfth thoracic vertebra, at the aortic hiatus in the diaphragm where it becomes the abdominal aorta.

The intercostal nerves are part of the somatic nervous system, and arise from the anterior rami of the thoracic spinal nerves from T1 to T11. The intercostal nerves are distributed chiefly to the thoracic pleura and abdominal peritoneum, and differ from the anterior rami of the other spinal nerves in that each pursues an independent course without plexus formation.

In human anatomy, the internal thoracic vein is the vein that drains the chest wall and breasts.

In human anatomy, the superior epigastric veins are two or more venae comitantes which accompany either superior epigastric artery before emptying into the internal thoracic vein. They participate in the drainage of the superior surface of the diaphragm.

The thyrocervical trunk is a short artery of the neck. It arises from the subclavian artery, then promptly divides into its branches: the inferior thyroid artery, suprascapular artery, and (sometimes) the transverse cervical artery.

The inferior phrenic artery is a bilaterally paired artery of the abdominal cavity which represents the main source of arterial supply to the diaphragm. Each artery usually arises either from the coeliac trunk or the abdominal aorta, however, their origin is highly variable and the different sites of origin are different for the left artery and right artery. The superior suprarenal artery is a branch of the inferior phrenic artery.
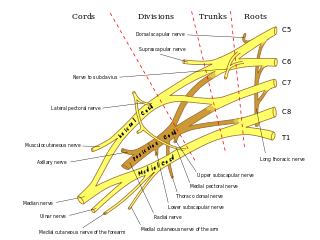
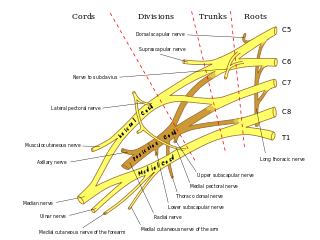
The subclavian nerve, also known as the nerve to the subclavius, is a small branch of the upper trunk of the brachial plexus. It contains axons from C5 and C6. It innervates the subclavius muscle.
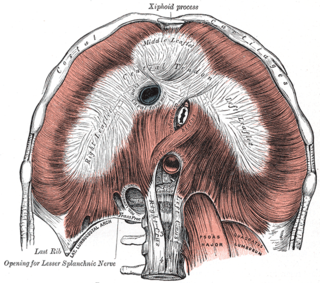
The central tendon of the diaphragm is a thin but strong aponeurosis situated slightly anterior to the vault formed by the muscle, resulting in longer posterior muscle fibers.
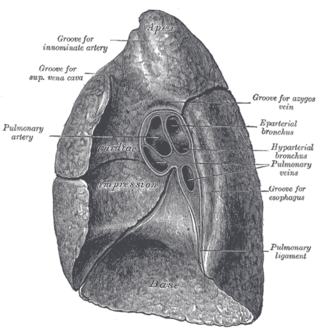
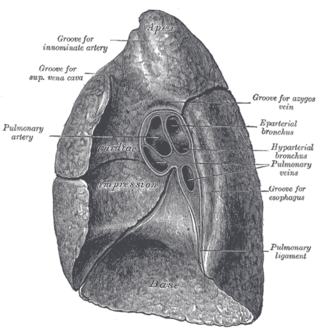
The root of the lung is a group of structures that emerge at the hilum of each lung, just above the middle of the mediastinal surface and behind the cardiac impression of the lung. It is nearer to the back than the front. The root of the lung is connected by the structures that form it to the heart and the trachea. The rib cage is separated from the lung by a two-layered membranous coating, the pleura. The hilum is the large triangular depression where the connection between the parietal pleura and the visceral pleura is made, and this marks the meeting point between the mediastinum and the pleural cavities.
The superior phrenic artery is a bilaterally paired artery of the thoracic cavity. The two arteries provide arterial supply to the superior surface of the diaphragm. Each artery typically arises from either the descending part of the thoracic aorta or the 10th intercostal artery. They are distributed to the posterior part of the superior surface of the diaphragm. They form anastomoses with the musculophrenic arteries, and pericardiacophrenic arteries.

The pulmonary pleurae are the two flattened sacs ensheathing each lung, locally appearing as two opposing layers of serous membrane separating the lungs from the mediastinum and the inside surfaces of the surrounding chest walls.