Related Research Articles

Caesarean section, also known as C-section, cesarean, or caesarean delivery, is the surgical procedure by which one or more babies are delivered through an incision in the mother's abdomen. It is often performed because vaginal delivery would put the mother or child at risk. Reasons for the operation include obstructed labor, twin pregnancy, high blood pressure in the mother, breech birth, shoulder presentation, and problems with the placenta or umbilical cord. A caesarean delivery may be performed based upon the shape of the mother's pelvis or history of a previous C-section. A trial of vaginal birth after C-section may be possible. The World Health Organization recommends that caesarean section be performed only when medically necessary.

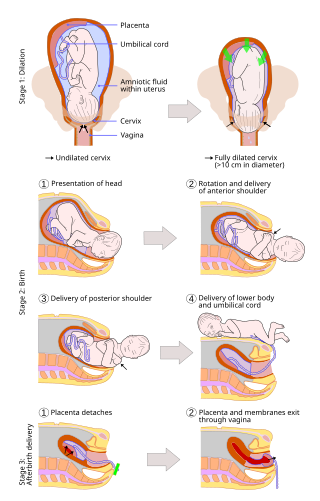
Childbirth, also known as labour, parturition and delivery, is the completion of pregnancy where one or more babies exits the internal environment of the mother via vaginal delivery or caesarean section. In 2019, there were about 140.11 million human births globally. In developed countries, most deliveries occur in hospitals, while in developing countries most are home births.

The postpartum period begins after childbirth and is typically considered to last for six weeks. There are three distinct phases of the postnatal period; the acute phase, lasting for six to twelve hours after birth; the subacute phase, lasting six weeks; and the delayed phase, lasting up to six months. During the delayed phase, some changes to the genitourinary system take much longer to resolve and may result in conditions such as urinary incontinence. The World Health Organization (WHO) describes the postnatal period as the most critical and yet the most neglected phase in the lives of mothers and babies; most maternal and newborn deaths occur during this period.

A breech birth is when a baby is born bottom first instead of head first, as is normal. Around 3–5% of pregnant women at term have a breech baby. Due to their higher than average rate of possible complications for the baby, breech births are generally considered higher risk. Breech births also occur in many other mammals such as dogs and horses, see veterinary obstetrics.
Labor induction is the process or treatment that stimulates childbirth and delivery. Inducing (starting) labor can be accomplished with pharmaceutical or non-pharmaceutical methods. In Western countries, it is estimated that one-quarter of pregnant women have their labor medically induced with drug treatment. Inductions are most often performed either with prostaglandin drug treatment alone, or with a combination of prostaglandin and intravenous oxytocin treatment.
A hysterotomy is an incision made in the uterus. This surgical incision is used in several medical procedures, including during termination of pregnancy in the second trimester and delivering the fetus during caesarean section. It is also used to gain access and perform surgery on a fetus during pregnancy to correct birth defects, and it is an option to achieve resuscitation if cardiac arrest occurs during pregnancy and it is necessary to remove the fetus from the uterus.

Placental abruption is when the placenta separates early from the uterus, in other words separates before childbirth. It occurs most commonly around 25 weeks of pregnancy. Symptoms may include vaginal bleeding, lower abdominal pain, and dangerously low blood pressure. Complications for the mother can include disseminated intravascular coagulopathy and kidney failure. Complications for the baby can include fetal distress, low birthweight, preterm delivery, and stillbirth.
Cervical dilation is the opening of the cervix, the entrance to the uterus, during childbirth, miscarriage, induced abortion, or gynecological surgery. Cervical dilation may occur naturally, or may be induced surgically or medically.

Uterine rupture is when the muscular wall of the uterus tears during pregnancy or childbirth. Symptoms, while classically including increased pain, vaginal bleeding, or a change in contractions, are not always present. Disability or death of the mother or baby may result.

Placenta accreta occurs when all or part of the placenta attaches abnormally to the myometrium. Three grades of abnormal placental attachment are defined according to the depth of attachment and invasion into the muscular layers of the uterus:
- Accreta – chorionic villi attached to the myometrium, rather than being restricted within the decidua basalis.
- Increta – chorionic villi invaded into the myometrium.
- Percreta – chorionic villi invaded through the perimetrium.
Caesarean delivery on maternal request (CDMR) is a caesarean section birth requested by the pregnant woman without a medical reason.
In case of a previous caesarean section a subsequent pregnancy can be planned beforehand to be delivered by either of the following two main methods:

Carbetocin, sold under the brand names Pabal among others, is a medication used to prevent excessive bleeding after childbirth, particularly following Cesarean section. It appears to work as well as oxytocin. Due to it being less economical than other options, use is not recommended by NHS Scotland. It is given by injection into a vein or muscle.
A vaginal delivery is the birth of offspring in mammals through the vagina. It is the most common method of childbirth worldwide. It is considered the preferred method of delivery, as it is correlated with lower morbidity and mortality than caesarean sections (C-sections), though it is not clear whether this is causal.
Pemberton v. Tallahassee Memorial Regional Center, 66 F. Supp. 2d 1247, is a case in the United States regarding reproductive rights. In particular, the case explored the limits of a woman's right to choose her medical treatment in light of fetal rights at the end of pregnancy.

In obstetrics, a shoulder presentation is a malpresentation at childbirth where the baby is in a transverse lie, thus the leading part is an arm, a shoulder, or the trunk. While a baby can be delivered vaginally when either the head or the feet/buttocks are the leading part, it usually cannot be expected to be delivered successfully with a shoulder presentation unless a cesarean section (C/S) is performed.
In obstetrics a trial of labour is the conduction of spontaneous labour in a moderate degree of cephalopelvic disproportion. It is performed under close observation by an obstetrician in order to assess a woman's chances of a successful vaginal birth. The physician may allow labor to continue against contraindications during birth or even stimulate labor with oxytocin when pelvic measurements are borderline to see if the fetal head will descend making vaginal delivery possible; if progressive changes in dilation and station do not occur, a cesarean delivery is performed.

Prolonged labor is the inability of a woman to proceed with childbirth upon going into labor. Prolonged labor typically lasts over 20 hours for first time mothers, and over 14 hours for women that have already had children. Failure to progress can take place during two different phases; the latent phase and active phase of labor. The latent phase of labor can be emotionally tiring and cause fatigue, but it typically does not result in further problems. The active phase of labor, on the other hand, if prolonged, can result in long term complications.
The Human Microbiome Project (HMP), completed in 2012, laid the foundation for further investigation into the role the microbiome plays in overall health and disease. One area of particular interest is the role which delivery mode plays in the development of the infant/neonate microbiome and what potential implications this may have long term. It has been found that infants born via vaginal delivery have microbiomes closely mirroring that of the mother's vaginal microbiome, whereas those born via cesarean section tend to resemble that of the mother's skin. One notable study from 2010 illustrated an abundance of Lactobacillus and other typical vaginal genera in stool samples of infants born via vaginal delivery and an abundance of Staphylococcus and Corynebacterium, commonly found on the skin surfaces, in stool samples of infants born via cesarean section. From these discoveries came the concept of vaginal seeding, also known as microbirthing, which is a procedure whereby vaginal fluids are applied to a new-born child delivered by caesarean section. The idea of vaginal seeding was explored in 2015 after Maria Gloria Dominguez-Bello discovered that birth by caesarean section significantly altered the newborn child's microbiome compared to that of natural birth. The purpose of the technique is to recreate the natural transfer of bacteria that the baby gets during a vaginal birth. It involves placing swabs in the mother's vagina, and then wiping them onto the baby's face, mouth, eyes and skin. Due to the long-drawn nature of studying the impact of vaginal seeding, there are a limited number of studies available that support or refute its use. The evidence suggests that applying microbes from the mother's vaginal canal to the baby after cesarean section may aid in the partial restoration of the infant's natural gut microbiome with an increased likelihood of pathogenic infection to the child via vertical transmission.

A uterine niche, also known as a Cesarean scar defect or an isthmocele, is an indentation of the myometrium at the site of a cesarean section with a depth of at least 2 mm.
References
- ↑ "Vaginal Birth After Cesarean Delivery - Deciding on a Trial of Labor After Cesarean Delivery - ACOG". www.acog.org. Retrieved 2016-05-29.
- ↑ "Vaginal birth after cesarean delivery (VBAC)". www.uptodate.com. Retrieved 2016-05-29.