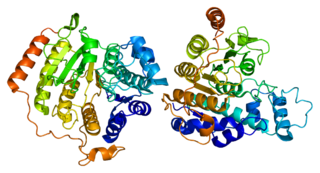
Histone deacetylases (EC 3.5.1.98, HDAC) are a class of enzymes that remove acetyl groups (O=C-CH3) from an ε-N-acetyl lysine amino acid on both histone and non-histone proteins. HDACs allow histones to wrap the DNA more tightly. This is important because DNA is wrapped around histones, and DNA expression is regulated by acetylation and de-acetylation. HDAC's action is opposite to that of histone acetyltransferase. HDAC proteins are now also called lysine deacetylases (KDAC), to describe their function rather than their target, which also includes non-histone proteins. In general, they suppress gene expression.

Cutaneous T-cell lymphoma (CTCL) is a class of non-Hodgkin lymphoma, which is a type of cancer of the immune system. Unlike most non-Hodgkin lymphomas, CTCL is caused by a mutation of T cells. The cancerous T cells in the body initially migrate to the skin, causing various lesions to appear. These lesions change shape as the disease progresses, typically beginning as what appears to be a rash which can be very itchy and eventually forming plaques and tumors before spreading to other parts of the body.

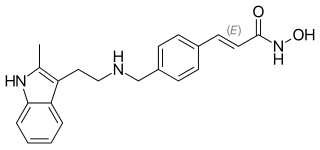
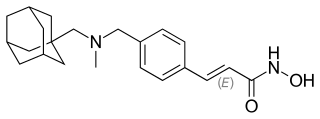
Trichostatin A (TSA) is an organic compound that serves as an antifungal antibiotic and selectively inhibits the class I and II mammalian histone deacetylase (HDAC) families of enzymes, but not class III HDACs. However, there are recent reports of the interactions of this molecule with Sirt 6 protein. TSA inhibits the eukaryotic cell cycle during the beginning of the growth stage. TSA can be used to alter gene expression by interfering with the removal of acetyl groups from histones and therefore altering the ability of DNA transcription factors to access the DNA molecules inside chromatin. It is a member of a larger class of histone deacetylase inhibitors that have a broad spectrum of epigenetic activities. Thus, TSA has some potential as an anti-cancer drug. One suggested mechanism is that TSA promotes the expression of apoptosis-related genes, leading to cancerous cells surviving at lower rates, thus slowing the progression of cancer. Other mechanisms may include the activity of HDIs to induce cell differentiation, thus acting to "mature" some of the de-differentiated cells found in tumors. HDIs have multiple effects on non-histone effector molecules, so the anti-cancer mechanisms are truly not understood at this time.

Histone acetylation and deacetylation are the processes by which the lysine residues within the N-terminal tail protruding from the histone core of the nucleosome are acetylated and deacetylated as part of gene regulation.

Acute myeloblastic leukemia with maturation (M2) is a subtype of acute myeloid leukemia (AML).
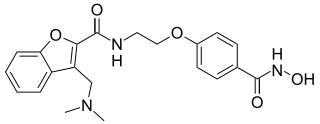
Histone deacetylase inhibitors are chemical compounds that inhibit histone deacetylases.
Chromatin remodeling is the dynamic modification of chromatin architecture to allow access of condensed genomic DNA to the regulatory transcription machinery proteins, and thereby control gene expression. Such remodeling is principally carried out by 1) covalent histone modifications by specific enzymes, e.g., histone acetyltransferases (HATs), deacetylases, methyltransferases, and kinases, and 2) ATP-dependent chromatin remodeling complexes which either move, eject or restructure nucleosomes. Besides actively regulating gene expression, dynamic remodeling of chromatin imparts an epigenetic regulatory role in several key biological processes, egg cells DNA replication and repair; apoptosis; chromosome segregation as well as development and pluripotency. Aberrations in chromatin remodeling proteins are found to be associated with human diseases, including cancer. Targeting chromatin remodeling pathways is currently evolving as a major therapeutic strategy in the treatment of several cancers.
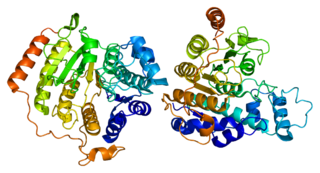
Histone deacetylase 8 is an enzyme that in humans is encoded by the HDAC8 gene.
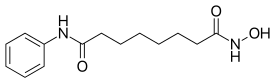
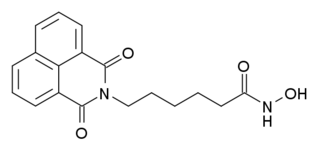
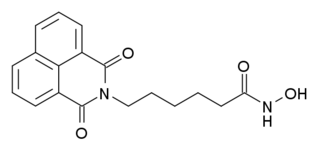
Panobinostat, sold under the brand name Farydak, is a medication used for the treatment of multiple myeloma. It is a hydroxamic acid and acts as a non-selective histone deacetylase inhibitor.

Romidepsin, sold under the brand name Istodax, is an anticancer agent used in cutaneous T-cell lymphoma (CTCL) and other peripheral T-cell lymphomas (PTCLs). Romidepsin is a natural product obtained from the bacterium Chromobacterium violaceum, and works by blocking enzymes known as histone deacetylases, thus inducing apoptosis. It is sometimes referred to as depsipeptide, after the class of molecules to which it belongs. Romidepsin is branded and owned by Gloucester Pharmaceuticals, a part of Celgene.
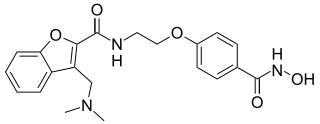
Givinostat (INN) or gavinostat is a histone deacetylase inhibitor with potential anti-inflammatory, anti-angiogenic, and antineoplastic activities. It is a hydroxamic acid used in the form of its hydrochloride.

Spiruchostatins are a group of chemical compounds isolated from Pseudomonas sp. as gene expression-enhancing substances. They possess novel bicyclic depsipeptides involving 4-amino-3-hydroxy-5-methylhexanoic acid and 4-amino-3-hydroxy-5-methylheptanoic acid residues. The two main forms are spiruchostatin A and spiruchostatin B.
Abexinostat is an experimental drug candidate for cancer treatment. It was developed by Pharmacyclics and licensed to Xynomic. and is in Phase II clinical trials for B-cell lymphoma. Pre-clinical study suggests the potential for treatment of different types of cancer as well.
Paul Alan Marks was a medical doctor, researcher and administrator. He was a faculty member and president at Memorial Sloan Kettering Cancer Center.

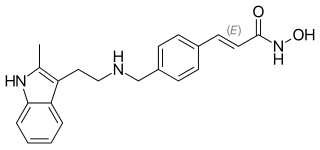
Pracinostat (SB939) is an orally bioavailable, small-molecule histone deacetylase (HDAC) inhibitor based on hydroxamic acid with potential anti-tumor activity characterized by favorable physicochemical, pharmaceutical, and pharmacokinetic properties.
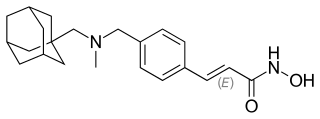
Martinostat is a histone deacetylase inhibitor (HDACi) that is potent against recombinant class I HDACs and class IIb HDAC with low nanomolar affinities. In tissue CETSA assays, martinostat exhibits selectivity for class I HDACs. When tagged with the radioisotope carbon-11, martinostat can be used to quantify HDAC in the brain and peripheral organs using positron emission tomography. Martinostat was given a name that adopted the style of other HDAC inhibitors, such as vorinostat, entinostat, and crebinostat, that recognized the academic center in which it was developed, the Martinos Center for Biomedical Imaging.
Scriptaid is a drug which acts as a histone deacetylase inhibitor, and was one of the first compounds discovered via high-throughput screening that acts at this target. Scriptaid itself was never developed for medical applications, but led to the development of structurally related drugs such as vorinostat, which have been accepted into clinical use. Most early research using these compounds focused on their anti-cancer activity, but more recent research has found scriptaid to be useful in other applications such as cloning and research into regulation of metabolism.
Richard Rifkind was an American cancer researcher.

Epigenetic priming is the modification to a cell's epigenome whereby specific chromatin domains within a cell are converted from a closed state to an open state, usually as the result of an external biological trigger or pathway, allowing for DNA access by transcription factors or other modification mechanisms. The action of epigenetic priming for a certain region of DNA dictates how other gene regulation mechanisms will be able to act on the DNA later in the cell’s life. Epigenetic priming has been chiefly investigated in neuroscience and cancer research, as it has been found to play a key role in memory formation within neurons and tumor-suppressor gene activation in cancer treatment respectively.

Zabadinostat is an experimental epigenetic drug being investigated as a potential treatment for advanced or metastatic cancers. It is an orally available Class I selective histone deacetylase (HDAC) inhibitor, with half maximal inhibitory concentrations (IC50) of 62 nM, 570 nM and 550 nM, against HDAC1, HDAC2 and HDAC3, respectively. It shows no activity against HDAC class II.