Related Research Articles

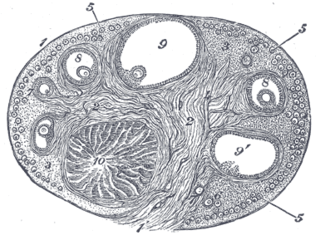
The ovary is an organ in the female reproductive system that produces an ovum. When released, this travels down the fallopian tube into the uterus. There is an ovary found on the left and the right side of the body. The ovaries also secrete hormones that play a role in the menstrual cycle and fertility. The ovary progresses through many stages beginning in the prenatal period through menopause. It is also an endocrine gland because of the various hormones that it secretes.

The human body is the structure of a human being. It is composed of many different types of cells that together create tissues and subsequently organs and then organ systems. They ensure homeostasis and the viability of the human body.

The menstrual cycle is a series of natural changes in hormone production and the structures of the uterus and ovaries of the female reproductive system that makes pregnancy possible. The ovarian cycle controls the production and release of eggs and the cyclic release of estrogen and progesterone. The uterine cycle governs the preparation and maintenance of the lining of the uterus (womb) to receive an embryo. These cycles are concurrent and coordinated, normally last between 21 and 35 days, with a median length of 28 days, and continue for about 30–45 years.

Ovulation is the release of eggs from the ovaries. In women, this event occurs when the ovarian follicles rupture and release the secondary oocyte ovarian cells. After ovulation, during the luteal phase, the egg will be available to be fertilized by sperm. In addition, the uterine lining (endometrium) is thickened to be able to receive a fertilized egg. If no conception occurs, the uterine lining as well as the egg will be shed during menstruation.
Luteinizing hormone is a hormone produced by gonadotropic cells in the anterior pituitary gland. The production of LH is regulated by gonadotropin-releasing hormone (GnRH) from the hypothalamus. In females, an acute rise of LH known as an LH surge, triggers ovulation and development of the corpus luteum. In males, where LH had also been called interstitial cell–stimulating hormone (ICSH), it stimulates Leydig cell production of testosterone. It acts synergistically with follicle-stimulating hormone (FSH).

An ovarian cyst is a fluid-filled sac within the ovary. Often they cause no symptoms. Occasionally they may produce bloating, lower abdominal pain, or lower back pain. The majority of cysts are harmless. If the cyst either breaks open or causes twisting of the ovary, it may cause severe pain. This may result in vomiting or feeling faint, and even cause head aches.
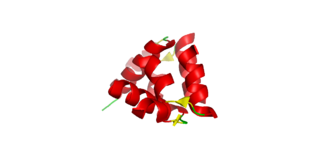
The corpus luteum is a temporary endocrine structure in female ovaries involved in the production of relatively high levels of progesterone, and moderate levels of estradiol, and inhibin A. It is the remains of the ovarian follicle that has released a mature ovum during a previous ovulation.

An ovarian follicle is a roughly spheroid cellular aggregation set found in the ovaries. It secretes hormones that influence stages of the menstrual cycle. At the time of puberty, those with ovaries have approximately 200,000 to 300,000 follicles, each with the potential to release an egg cell (ovum) at ovulation for fertilization. These eggs are developed once every menstrual cycle with around 450–500 being ovulated during a woman's reproductive lifetime.

The corpus albicans is the regressed form of the corpus luteum. As the corpus luteum is being broken down by macrophages, fibroblasts lay down type I collagen, forming the corpus albicans. This process is called "luteolysis". The remains of the corpus albicans may persist as a scar on the surface of the ovary.

A stigma, also called macula pellucida, in mammalian reproductive anatomy, refers to the area of the ovarian surface where the Graafian follicle will burst through during ovulation and release the ovum. As the follicle matures, the area between the follicle and the ovarian surface begins to thin and weaken under the influence of the luteinizing hormone and local cytokines. At ovulation the stigma ruptures and the secondary oocyte is released along with surrounding granulosa cells, from the region of the cumulus oophorus, and follicular fluid. The secondary oocyte needs to be captured by the fallopian tube where it could be fertilized by a sperm cell. The stigma will heal and the residual follicle is transformed into the corpus luteum.
In mammalian species, pseudopregnancy is a physical state whereby all the signs and symptoms of pregnancy are exhibited, with the exception of the presence of a fetus, creating a false pregnancy. The corpus luteum is responsible for the development of maternal behavior and lactation, which are mediated by the continued production of progesterone by the corpus luteum through some or all of pregnancy. In most species, the corpus luteum is degraded in the absence of a pregnancy. However, in some species, the corpus luteum may persist in the absence of pregnancy and cause "pseudopregnancy", in which the female will exhibit clinical signs of pregnancy.
The estrous cycle is a set of recurring physiological changes induced by reproductive hormones in females of mammalian subclass Theria. Estrous cycles start after sexual maturity in females and are interrupted by anestrous phases, otherwise known as "rest" phases, or by pregnancies. Typically, estrous cycles repeat until death. These cycles are widely variable in duration and frequency depending on the species. Some animals may display bloody vaginal discharge, often mistaken for menstruation. Many mammals used in commercial agriculture, such as cattle and sheep, may have their estrous cycles artificially controlled with hormonal medications for optimum productivity. The male equivalent, seen primarily in ruminants, is called rut.

In biology, folliculogenesis is the maturation of the ovarian follicle, a densely packed shell of somatic cells that contains an immature oocyte. Folliculogenesis describes the progression of a number of small primordial follicles into large preovulatory follicles that occurs in part during the menstrual cycle.
Luteolysis is the structural and functional degradation of the corpus luteum, which occurs at the end of the luteal phase of both the estrous and menstrual cycles in the absence of pregnancy.

The menstrual cycle is on average 28 days in length. It begins with menses during the follicular phase and followed by ovulation and ending with the luteal phase. Unlike the follicular phase which can vary in length among individuals, the luteal phase is typically fixed at approximately 14 days and is characterized by changes to hormone levels, such as an increase in progesterone and estrogen levels, decrease in gonadotropins such as follicle-stimulating hormone (FSH) and luteinizing hormone (LH), changes to the endometrial lining to promote implantation of the fertilized egg, and development of the corpus luteum. In the absence of fertilization by sperm, the corpus luteum atrophies leading to a decrease in progesterone and estrogen, an increase in FSH and LH, and shedding of the endometrial lining (menses) to begin the menstrual cycle again.
Relaxin is a protein hormone of about 6000 Da, first described in 1926 by Frederick Hisaw.
Theca interna cells express receptors for luteinizing hormone (LH) to produce androstenedione, which via a few steps, gives the granulosa the precursor for estrogen manufacturing.
The theca folliculi comprise a layer of the ovarian follicles. They appear as the follicles become secondary follicles.

A corpus luteum cyst is a type of ovarian cyst which may rupture about the time of menstruation, and take up to three months to disappear entirely. A corpus luteum cyst rarely occurs in women over the age of 50, because eggs are no longer being released after menopause. Corpus luteum cysts may contain blood and other fluids. The physical shape of a corpus luteum cyst may appear as an enlargement of the ovary itself, rather than a distinct mass -like growth on the surface of the ovary.
Ovarian apoplexy is a sudden rupture in the ovary, commonly at the site of a cyst, accompanied by hemorrhage in the ovarian tissue and/or intraperitoneal bleeding.
References
- ↑ McSweeney, Daniel J.; Wood, Frank O. (1940). "Acute Abdominal Conditions Following Ovulation and Its Sequelae". New England Journal of Medicine. 222 (5): 174–179. doi:10.1056/NEJM194002012220502.
- ↑ Marieb, Elaine (2013). Anatomy & physiology. Benjamin-Cummings. p. 915. ISBN 9780321887603.
- ↑ Husvéth, Ferenc (2011). "PHYSIOLOGICAL and REPRODUCTIONAL ASPECTS OF ANIMAL PRODUCTION". Digital Textbook Library. Debreceni Egyetem. Retrieved 4 July 2015.