The endometrium is the inner epithelial layer, along with its mucous membrane, of the mammalian uterus. It has a basal layer and a functional layer: the basal layer contains stem cells which regenerate the functional layer. The functional layer thickens and then is shed during menstruation in humans and some other mammals, including other apes, Old World monkeys, some species of bat, the elephant shrew and the Cairo spiny mouse. In most other mammals, the endometrium is reabsorbed in the estrous cycle. During pregnancy, the glands and blood vessels in the endometrium further increase in size and number. Vascular spaces fuse and become interconnected, forming the placenta, which supplies oxygen and nutrition to the embryo and fetus. The speculated presence of an endometrial microbiota has been argued against.

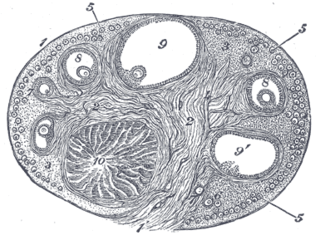
The ovary is a gonad in the female reproductive system that produces ova; when released, an ovum travels through the fallopian tube/oviduct into the uterus. There is an ovary on the left and the right side of the body. The ovaries are endocrine glands, secreting various hormones that play a role in the menstrual cycle and fertility. The ovary progresses through many stages beginning in the prenatal period through menopause.
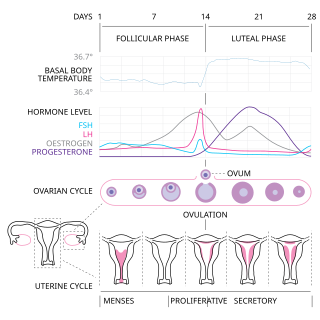
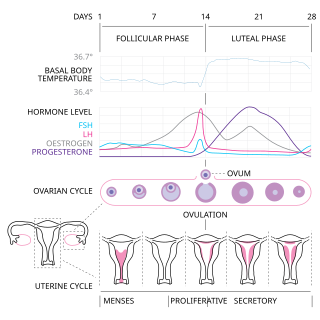
The menstrual cycle is a series of natural changes in hormone production and the structures of the uterus and ovaries of the female reproductive system that makes pregnancy possible. The ovarian cycle controls the production and release of eggs and the cyclic release of estrogen and progesterone. The uterine cycle governs the preparation and maintenance of the lining of the uterus (womb) to receive an embryo. These cycles are concurrent and coordinated, normally last between 21 and 35 days, with a median length of 28 days. Menarche usually occurs around the age of 12 years; menstrual cycles continue for about 30–45 years.

Ovulation is an important part of the menstrual cycle in female vertebrates where the egg cells are released from the ovaries as part of the ovarian cycle. In human females ovulation typically occurs near the midpoint in the menstrual cycle and after the follicular phase. Ovulation is stimulated by an increase in luteinizing hormone (LH). The ovarian follicles rupture and release the secondary oocyte ovarian cells.

Progestogens, also sometimes written progestins, progestagens or gestagens, are a class of natural or synthetic steroid hormones that bind to and activate the progesterone receptors (PR). Progesterone is the major and most important progestogen in the body. The progestogens are named for their function in maintaining pregnancy, although they are also present at other phases of the estrous and menstrual cycles.
Luteinizing hormone is a hormone produced by gonadotropic cells in the anterior pituitary gland. The production of LH is regulated by gonadotropin-releasing hormone (GnRH) from the hypothalamus. In females, an acute rise of LH known as an LH surge, triggers ovulation and development of the corpus luteum. In males, where LH had also been called interstitial cell–stimulating hormone (ICSH), it stimulates Leydig cell production of testosterone. It acts synergistically with follicle-stimulating hormone (FSH).
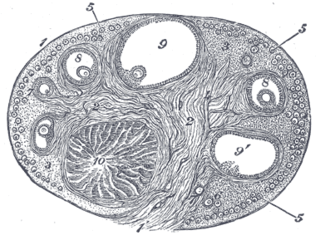
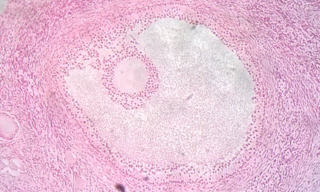
The corpus luteum is a temporary endocrine structure in female ovaries involved in the production of relatively high levels of progesterone, and moderate levels of estradiol, and inhibin A. It is the remains of the ovarian follicle that has released a mature ovum during a previous ovulation.

Oogenesis or ovogenesis is the differentiation of the ovum into a cell competent to further develop when fertilized. It is developed from the primary oocyte by maturation. Oogenesis is initiated in the embryonic stage.

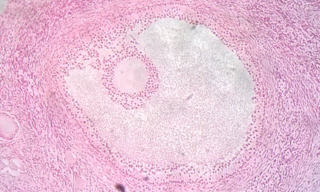
An ovarian follicle is a roughly spheroid cellular aggregation set found in the ovaries. It secretes hormones that influence stages of the menstrual cycle. At the time of puberty, women have approximately 200,000 to 300,000 follicles, each with the potential to release an egg cell (ovum) at ovulation for fertilization. These eggs are developed once every menstrual cycle with around 450–500 being ovulated during a woman's reproductive lifetime.

A granulosa cell or follicular cell is a somatic cell of the sex cord that is closely associated with the developing female gamete in the ovary of mammals.
In mammalian species, pseudopregnancy is a physical state whereby all the signs and symptoms of pregnancy are exhibited, with the exception of the presence of a fetus, creating a false pregnancy. The corpus luteum is responsible for the development of maternal behavior and lactation, which are mediated by the continued production of progesterone by the corpus luteum through some or all of pregnancy. In most species, the corpus luteum is degraded in the absence of a pregnancy. However, in some species, the corpus luteum may persist in the absence of pregnancy and cause "pseudopregnancy", in which the female will exhibit clinical signs of pregnancy.
The estrous cycle is a set of recurring physiological changes induced by reproductive hormones in females of mammalian subclass Theria. Estrous cycles start after sexual maturity in females and are interrupted by anestrous phases, otherwise known as "rest" phases, or by pregnancies. Typically, estrous cycles repeat until death. These cycles are widely variable in duration and frequency depending on the species. Some animals may display bloody vaginal discharge, often mistaken for menstruation. Many mammals used in commercial agriculture, such as cattle and sheep, may have their estrous cycles artificially controlled with hormonal medications for optimum productivity. The male equivalent, seen primarily in ruminants, is called rut.

In biology, folliculogenesis is the maturation of the ovarian follicle, a densely packed shell of somatic cells that contains an immature oocyte. Folliculogenesis describes the progression of a number of small primordial follicles into large preovulatory follicles that occurs in part during the menstrual cycle.
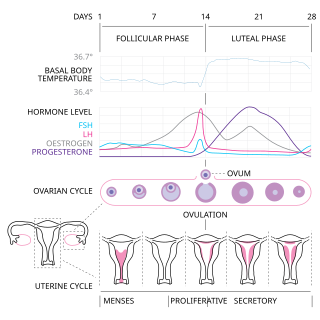
The menstrual cycle is on average 28 days in length. It begins with menses during the follicular phase, followed by ovulation and ending with the luteal phase. Unlike the follicular phase which can vary in length among individuals, the luteal phase is typically fixed at approximately 14 days and is characterized by changes to hormone levels, such as an increase in progesterone and estrogen levels, decrease in gonadotropins such as follicle-stimulating hormone (FSH) and luteinizing hormone (LH), changes to the endometrial lining to promote implantation of the fertilized egg, and development of the corpus luteum. In the absence of fertilization by sperm, the corpus luteum degenerates leading to a decrease in progesterone and estrogen, an increase in FSH and LH, and shedding of the endometrial lining (menses) to begin the menstrual cycle again.
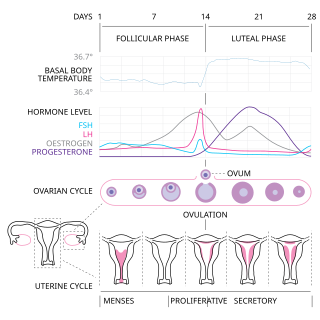
The follicular phase, also known as the preovulatory phase or proliferative phase, is the phase of the estrous cycle during which follicles in the ovary mature from primary follicle to a fully mature graafian follicle. It ends with ovulation. The main hormones controlling this stage are secretion of gonadotropin-releasing hormones, which are follicle-stimulating hormones and luteinising hormones. They are released by pulsatile secretion. The duration of the follicular phase can differ depending on the length of the menstrual cycle, while the luteal phase is usually stable, does not really change and lasts 14 days.
Follicular atresia refers to the process in which a follicle fails to develop, thus preventing it from ovulating and releasing an egg. It is a normal, naturally occurring progression that occurs as mammalian ovaries age. Approximately 1% of mammalian follicles in ovaries undergo ovulation and the remaining 99% of follicles go through follicular atresia as they cycle through the growth phases. In summary, follicular atresia is a process that leads to the follicular loss and loss of oocytes, and any disturbance or loss of functionality of this process can lead to many other conditions.
Theca interna cells express receptors for luteinizing hormone (LH) to produce androstenedione, which via a few steps, gives the granulosa the precursor for estrogen manufacturing.
The theca folliculi comprise a layer of the ovarian follicles. They appear as the follicles become secondary follicles.

A corpus luteum cyst or luteal cyst is a type of ovarian cyst which may rupture about the time of menstruation, and take up to three months to disappear entirely. A corpus luteum cyst does not often occur in women over the age of 50, because eggs are no longer being released after menopause. Corpus luteum cysts may contain blood and other fluids. The physical shape of a corpus luteum cyst may appear as an enlargement of the ovary itself, rather than a distinct mass-like growth on the surface of the ovary.
Hormones during pregnancy are the result of an intricate interaction between hormones generated by different glands and organs. The primary hormones involved comprise human chorionic gonadotropin (hCG), progesterone, estrogen, human placental lactogen (hPL), and oxytocin. Hormones are synthesized in certain organs, including the ovaries, placenta, and pituitary gland. These hormones have essential functions in pregnancy test, maintaining the uterine lining, fetal development, preventing premature labor, and the initiation and support of labor.