Related Research Articles

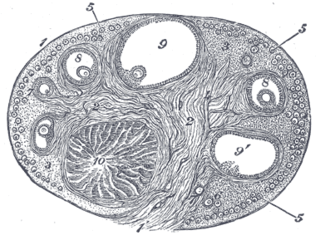
The ovary is a gonad in the female reproductive system that produces ova; when released, an ovum travels through the fallopian tube/oviduct into the uterus. There is an ovary on the left and the right side of the body. The ovaries are endocrine glands, secreting various hormones that play a role in the menstrual cycle and fertility. The ovary progresses through many stages beginning in the prenatal period through menopause.
The corpus luteum is a temporary endocrine structure in female ovaries involved in the production of relatively high levels of progesterone, and moderate levels of estradiol, and inhibin A. It is the remains of the ovarian follicle that has released a mature ovum during a previous ovulation.

An ovarian follicle is a roughly spheroid cellular aggregation set found in the ovaries. It secretes hormones that influence stages of the menstrual cycle. At the time of puberty, women have approximately 200,000 to 300,000 follicles, each with the potential to release an egg cell (ovum) at ovulation for fertilization. These eggs are developed once every menstrual cycle with around 450–500 being ovulated during a woman's reproductive lifetime.

The corpus albicans is the regressed form of the corpus luteum. As the corpus luteum is being broken down by macrophages, fibroblasts lay down type I collagen, forming the corpus albicans. This process is called "luteolysis". The remains of the corpus albicans may persist as a scar on the surface of the ovary.

The zona pellucida is the specialized area surrounding mammalian oocytes (eggs). It is also known as an egg coat. The zona pellucida is essential for oocyte growth and fertilization.

A granulosa cell or follicular cell is a somatic cell of the sex cord that is closely associated with the developing female gamete in the ovary of mammals.
The efferent ducts connect the rete testis with the initial section of the epididymis.

The adventitia is the outer layer of fibrous connective tissue surrounding an organ.

In biology, folliculogenesis is the maturation of the ovarian follicle, a densely packed shell of somatic cells that contains an immature oocyte. Folliculogenesis describes the progression of a number of small primordial follicles into large preovulatory follicles that occurs in part during the menstrual cycle.

Dense connective tissue, also called dense fibrous tissue, is a type of connective tissue with fibers as its main matrix element. The fibers are mainly composed of type I collagen. Crowded between the collagen fibers are rows of fibroblasts, fiber-forming cells, that generate the fibers. Dense connective tissue forms strong, rope-like structures such as tendons and ligaments. Tendons attach skeletal muscles to bones; ligaments connect bones to bones at joints. Ligaments are more stretchy and contain more elastic fibers than tendons. Dense connective tissue also make up the lower layers of the skin (dermis), where it is arranged in sheets. In addition, the sclera contains dense connective tissue

The broad ligament of the uterus is the wide fold of peritoneum that connects the sides of the uterus to the walls and floor of the pelvis.

In anatomy and physiology, a duct is a circumscribed channel leading from an exocrine gland or organ.

The perimetrium is the outer serosal layer of the uterus, derived from the peritoneum overlying the uterine fundus, and can be considered a visceral peritoneum. It consists of a superficial layer of mesothelium, and a thin layer of loose connective tissue beneath it.
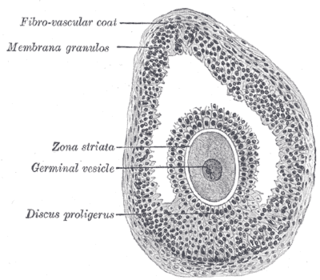
The cumulus oophorus is a cluster of cells that surround the oocyte both in the ovarian follicle and after ovulation. In the antral follicle, it may be regarded as an extension of the membrana granulosa. The innermost layer of these cells is the corona radiata.
The theca folliculi comprise a layer of the ovarian follicles. They appear as the follicles become secondary follicles.
The follicular antrum is the portion of an ovarian follicle filled with follicular fluid. Appearance of the follicular antrum during follicular maturation is the first sign that a follicle has reached the next stage of maturation. It has changed from a primary follicle to a secondary follicle.

Uterine glands or endometrial glands are tubular glands, lined by a simple columnar epithelium, found in the functional layer of the endometrium that lines the uterus. Their appearance varies during the menstrual cycle. During the proliferative phase, uterine glands appear long due to estrogen secretion by the ovaries. During the secretory phase, the uterine glands become very coiled with wide lumens and produce a glycogen-rich secretion known as histotroph or uterine milk. This change corresponds with an increase in blood flow to spiral arteries due to increased progesterone secretion from the corpus luteum. During the pre-menstrual phase, progesterone secretion decreases as the corpus luteum degenerates, which results in decreased blood flow to the spiral arteries. The functional layer of the uterus containing the glands becomes necrotic, and eventually sloughs off during the menstrual phase of the cycle.

The uterine horns are the points in the upper uterus where the fallopian tubes or oviducts exit to meet the ovaries. They are one of the points of attachment for the round ligament of uterus. They also provide attachment to the ovarian ligament, which is located below the fallopian tube at the back, while the round ligament of uterus is located below the tube at the front.
The theca externa is the outer layer of the theca folliculi. It is derived from connective tissue, the cells resembling fibroblasts, and contains abundant collagen. During ovulation, the surge in luteinizing hormone increases cAMP which increases progesterone and PGF2α production. The PGF2α induces the contraction of the smooth muscle cells of the theca externa, increasing intrafollicular pressure. This aids in rupture of the mature oocyte, or immature oocyte at the germinal vesicle stage in the canine, along with plasmin and collagenase degradation of the follicle wall.
Theca lutein cyst is a type of bilateral functional ovarian cyst filled with clear, straw-colored fluid. These cysts result from exaggerated physiological stimulation due to elevated levels of beta-human chorionic gonadotropin (beta-hCG) or hypersensitivity to beta-hCG. On ultrasound and MRI, theca lutein cysts appear in multiples on ovaries that are enlarged.
References
- ↑ Takei, Yoshio; Ando, Hironori; Tsutsui, Kazuyoshi (2016). "Subchapter 94G - Estradiol-17β". Handbook of hormones: comparative endocrinology for basic and clinical research. Nihon Hikaku Naibunpi Gakkai (1st ed.). Oxford: Elsevier, Academic Press. pp. 520–522. doi:10.1016/B978-0-12-801028-0.00226-9. ISBN 978-0-12-801028-0.
- 1 2 The IUPS Physiome Project --> Female Reproductive System - Cells Archived December 10, 2009, at the Wayback Machine Retrieved on Nov 9, 2009