Related Research Articles

A microorganism, or microbe, is an organism of microscopic size, which may exist in its single-celled form or as a colony of cells.

An infection is the invasion of tissues by pathogens, their multiplication, and the reaction of host tissues to the infectious agent and the toxins they produce. An infectious disease, also known as a transmissible disease or communicable disease, is an illness resulting from an infection.

Koch's postulates are four criteria designed to establish a causal relationship between a microbe and a disease. The postulates were formulated by Robert Koch and Friedrich Loeffler in 1884, based on earlier concepts described by Jakob Henle, and the statements were refined and published by Koch in 1890. Koch applied the postulates to describe the etiology of cholera and tuberculosis, both of which are now ascribed to bacteria. The postulates have been controversially generalized to other diseases. More modern concepts in microbial pathogenesis cannot be examined using Koch's postulates, including viruses and asymptomatic carriers. They have largely been supplanted by other criteria such as the Bradford Hill criteria for infectious disease causality in modern public health and the Molecular Koch's postulates for microbial pathogenesis.
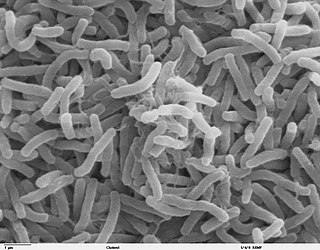
The germ theory of disease is the currently accepted scientific theory for many diseases. It states that microorganisms known as pathogens or "germs" can affect disease. These small organisms, too small to be seen without magnification, invade humans, other animals, and other living hosts. Their growth and reproduction within their hosts can cause disease. "Germ" refers to not just a bacterium but to any type of microorganism, such as protists or fungi, or even non-living pathogens that can cause disease, such as viruses, prions, or viroids. Diseases caused by pathogens are called infectious diseases. Even when a pathogen is the principal cause of a disease, environmental and hereditary factors often influence the severity of the disease, and whether a potential host individual becomes infected when exposed to the pathogen. Pathogens are disease-carrying agents that can pass from one individual to another, both in humans and animals. Infectious diseases are caused by biological agents such as pathogenic microorganisms as well as parasites.
Pathophysiology is a branch of study, at the intersection of pathology and physiology, concerning disordered physiological processes that cause, result from, or are otherwise associated with a disease or injury. Pathology is the medical discipline that describes conditions typically observed during a disease state, whereas physiology is the biological discipline that describes processes or mechanisms operating within an organism. Pathology describes the abnormal or undesired condition, whereas pathophysiology seeks to explain the functional changes that are occurring within an individual due to a disease or pathologic state.
In molecular biology, a hybridization probe(HP) is a fragment of DNA or RNA of usually 15–10000 nucleotide long which can be radioactively or fluorescently labeled. HP can be used to detect the presence of nucleotide sequences in analyzed RNA or DNA that are complementary to the sequence in the probe. The labeled probe is first denatured (by heating or under alkaline conditions such as exposure to sodium hydroxide) into single stranded DNA (ssDNA) and then hybridized to the target ssDNA (Southern blotting) or RNA (northern blotting) immobilized on a membrane or in situ.

Stanley "Stan" Falkow was an American microbiologist and a professor of microbiology at Georgetown University, University of Washington, and Stanford University School of Medicine. Falkow is known as the father of the field of molecular microbial pathogenesis. He formulated molecular Koch's postulates, which have guided the study of the microbial determinants of infectious diseases since the late 1980s. Falkow spent over 50 years uncovering molecular mechanisms of how bacteria cause disease and how to disarm them. Falkow also was one of the first scientists to investigate antimicrobial resistance, and presented his research extensively to scientific, government, and lay audiences explaining the spread of resistance from one organism to another, now known as horizontal gene transfer, and the implications of this phenomenon on our ability to combat infections in the future.

Food microbiology is the study of the microorganisms that inhabit, create, or contaminate food. This includes the study of microorganisms causing food spoilage; pathogens that may cause disease ; microbes used to produce fermented foods such as cheese, yogurt, bread, beer, and wine; and microbes with other useful roles, such as producing probiotics.
Molecular Koch's postulates are a set of experimental criteria that must be satisfied to show that a gene found in a pathogenic microorganism encodes a product that contributes to the disease caused by the pathogen. Genes that satisfy molecular Koch's postulates are often referred to as virulence factors. The postulates were formulated by the microbiologist Stanley Falkow in 1988 and are based on Koch's postulates.

Medical microbiology, the large subset of microbiology that is applied to medicine, is a branch of medical science concerned with the prevention, diagnosis and treatment of infectious diseases. In addition, this field of science studies various clinical applications of microbes for the improvement of health. There are four kinds of microorganisms that cause infectious disease: bacteria, fungi, parasites and viruses, and one type of infectious protein called prion.

Oral microbiology is the study of the microorganisms (microbiota) of the oral cavity and their interactions between oral microorganisms or with the host. The environment present in the human mouth is suited to the growth of characteristic microorganisms found there. It provides a source of water and nutrients, as well as a moderate temperature. Resident microbes of the mouth adhere to the teeth and gums to resist mechanical flushing from the mouth to stomach where acid-sensitive microbes are destroyed by hydrochloric acid.

Microbiology is the scientific study of microorganisms, those being of unicellular (single-celled), multicellular, or acellular. Microbiology encompasses numerous sub-disciplines including virology, bacteriology, protistology, mycology, immunology, and parasitology.
The Bradford Hill criteria, otherwise known as Hill's criteria for causation, are a group of nine principles that can be useful in establishing epidemiologic evidence of a causal relationship between a presumed cause and an observed effect and have been widely used in public health research. They were established in 1965 by the English epidemiologist Sir Austin Bradford Hill.
The Selman A. Waksman Award in Microbiology is awarded by the U.S. National Academy of Sciences "in recognition of excellence in the field of microbiology." Named after Selman Waksman, it was first awarded in 1968. A $5000 prize is included in the honor.
Cause, also known as etiology and aetiology, is the reason or origination of something.
In biology, a pathogen, in the oldest and broadest sense, is any organism or agent that can produce disease. A pathogen may also be referred to as an infectious agent, or simply a germ.

David Arnold Relman is an American microbiologist and the Thomas C. and Joan M. Merigan Professor in Medicine, and in Microbiology & Immunology at the Stanford University School of Medicine. His research focuses on the human microbiome and microbial ecosystem—for which he was a pioneer in the use of modern molecular methods, as well as on pathogen discovery and the genomics of host response.

The branches of microbiology can be classified into pure and applied sciences. Microbiology can be also classified based on taxonomy, in the cases of bacteriology, mycology, protozoology, and phycology. There is considerable overlap between the specific branches of microbiology with each other and with other disciplines, and certain aspects of these branches can extend beyond the traditional scope of microbiology In general the field of microbiology can be divided in the more fundamental branch and the applied microbiology (biotechnology). In the more fundamental field the organisms are studied as the subject itself on a deeper (theoretical) level. Applied microbiology refers to the fields where the micro-organisms are applied in certain processes such as brewing or fermentation. The organisms itself are often not studied as such, but applied to sustain certain processes.
Clinical metagenomic next-generation sequencing (mNGS) is the comprehensive analysis of microbial and host genetic material in clinical samples from patients by next-generation sequencing. It uses the techniques of metagenomics to identify and characterize the genome of bacteria, fungi, parasites, and viruses without the need for a prior knowledge of a specific pathogen directly from clinical specimens. The capacity to detect all the potential pathogens in a sample makes metagenomic next generation sequencing a potent tool in the diagnosis of infectious disease especially when other more directed assays, such as PCR, fail. Its limitations include clinical utility, laboratory validity, sense and sensitivity, cost and regulatory considerations.

Sigmund Socransky was born on December 2, 1934, in Toronto, Canada. He received his DDS degree from the University of Toronto in 1957. Socransky studied microbiology and Periodontology at Harvard, receiving a certificate in 1961. That same year he was recruited to work as a research associate at the Forsyth Dental Center. In 1968, he was nominated Senior Member of the Staff and Head of the Department of Periodontology. During his 50-year career at Forsyth, he published over 300 manuscripts. His career focus was in the fields of Periodontology and oral microbiology. Socransky died on August 27, 2011 in Boston Massachusetts.
References
- ↑ Falkow S (1988). "Molecular Koch's postulates applied to microbial pathogenicity". Rev. Infect. Dis. 10 (Suppl 2): S274–6. doi:10.1093/cid/10.Supplement_2.S274. PMID 3055197.
- 1 2 3 Fredricks, David; Relman, David (January 1996). "Sequence-Based Identification of Microbial Pathogens: a Reconsideration of Koch's Postulates". Clinical Microbiology Reviews. 9 (1): 18–33. doi:10.1128/CMR.9.1.18. PMC 172879 . PMID 8665474.
- ↑ The seven points enumerated here are "paraphrases" of the original material, whose seven points are itemized in roman numerals for ease of reference, see p.30 in original