Mastectomy is the medical term for the surgical removal of one or both breasts, partially or completely. A mastectomy is usually carried out to treat breast cancer. In some cases, women believed to be at high risk of breast cancer have the operation as a preventive measure. Alternatively, some women can choose to have a wide local excision, also known as a lumpectomy, an operation in which a small volume of breast tissue containing the tumor and a surrounding margin of healthy tissue is removed to conserve the breast. Both mastectomy and lumpectomy are referred to as "local therapies" for breast cancer, targeting the area of the tumor, as opposed to systemic therapies, such as chemotherapy, hormonal therapy, or immunotherapy.

Nipple discharge is fluid from the nipple, with or without squeezing the breast. The discharge can be milky, clear, green, purulent, bloody, or faintly yellow. The consistency can be thick, thin, sticky, or watery.

Lumpectomy is a surgical removal of a discrete portion or "lump" of breast tissue, usually in the treatment of a malignant tumor or breast cancer. It is considered a viable breast conservation therapy, as the amount of tissue removed is limited compared to a full-breast mastectomy, and thus may have physical and emotional advantages over more disfiguring treatment. Sometimes a lumpectomy may be used to either confirm or rule out that cancer has actually been detected. A lumpectomy is usually recommended to patients whose cancer has been detected early and who do not have enlarged tumors. Although a lumpectomy is used to allow for most of the breast to remain intact, the procedure may result in adverse affects that can include sensitivity and result in scar tissue, pain, and possible disfiguration of the breast if the lump taken out is significant. According to National Comprehensive Cancer Network guidelines, lumpectomy may be performed for ductal carcinoma in situ (DCIS), invasive ductal carcinoma, or other conditions.

A papilloma is a benign epithelial tumor growing exophytically in nipple-like and often finger-like fronds. In this context, papilla refers to the projection created by the tumor, not a tumor on an already existing papilla.
The International Classification of Diseases for Oncology (ICD-O) is a domain-specific extension of the International Statistical Classification of Diseases and Related Health Problems for tumor diseases. This classification is widely used by cancer registries.

Lactiferous ducts are ducts that converge and form a branched system connecting the nipple to the lobules of the mammary gland. When lactogenesis occurs, under the influence of hormones, the milk is moved to the nipple by the action of smooth muscle contractions along the ductal system to the tip of the nipple. They are also referred to as galactophores, galactophorous ducts, mammary ducts, mamillary ducts or milk ducts.

Ductal carcinoma in situ (DCIS), also known as intraductal carcinoma, is a pre-cancerous or non-invasive cancerous lesion of the breast. DCIS is classified as Stage 0. It rarely produces symptoms or a breast lump one can feel, typically being detected through screening mammography. It has been diagnosed in a significant percentage of men.

Salivary gland tumours, also known as mucous gland adenomas or neoplasms, are tumours that form in the tissues of salivary glands. The salivary glands are classified as major or minor. The major salivary glands consist of the parotid, submandibular, and sublingual glands. The minor salivary glands consist of 800 to 1000 small mucus-secreting glands located throughout the lining of the oral cavity. Patients with these types of tumours may be asymptomatic.
Florid cutaneous papillomatosis (FCP), is an obligate paraneoplastic syndrome.

Lobular carcinoma in situ (LCIS) is an incidental microscopic finding with characteristic cellular morphology and multifocal tissue patterns. The condition is a laboratory diagnosis and refers to unusual cells in the lobules of the breast. The lobules and acini of the terminal duct-lobular unit (TDLU), the basic functional unit of the breast, may become distorted and undergo expansion due to the abnormal proliferation of cells comprising the structure. These changes represent a spectrum of atypical epithelial lesions that are broadly referred to as lobular neoplasia (LN).

Atypical ductal hyperplasia (ADH) is the term used for a benign lesion of the breast that indicates an increased risk of breast cancer.
Also called Zuska's disease, subareolar abscess is a subcutaneous abscess of the breast tissue beneath the areola of the nipple. It is a frequently aseptic inflammation and has been associated with squamous metaplasia of lactiferous ducts.
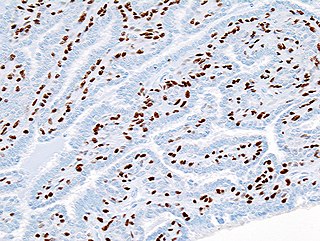
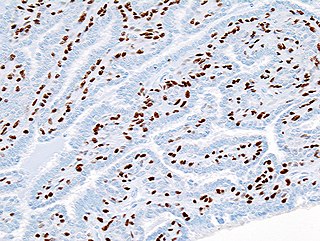
Intraductal papillomas of the breast are benign lesions with an incidence of approximately 2-3% in humans. They result from abnormal proliferation of the epithelial cells lining the breast ducts.

A breast mass, also known as a breast lump, is a localized swelling that feels different from the surrounding tissue. Breast pain, nipple discharge, or skin changes may be present. Concerning findings include masses that are hard, do not move easily, are of an irregular shape, or are firmly attached to surrounding tissue.

A cyst of Montgomery is a benign breast mass, usually found in adolescent girls. Typically, it resolves spontaneously by itself.

Galactography or ductography is a medical diagnostic procedure for viewing the milk ducts. The procedure involves the radiography of the ducts after injection of a radiopaque substance into the duct system through the nipple. The procedure is used for investigating the pathology of nipple discharge.
Microdochectomy is the surgical removal (excision) of a lactiferous duct. A mere incision of a mammary duct is called microdochotomy.
Central duct excision is the surgical removal (excision) of all lactiferous duct under the nipple. The excision of a single duct is called microdochectomy, a mere incision of a mammary duct is microdochotomy.
Papillomatosis of the breast (PB) is a rare, benign, epitheliosis-like lesion, i.e. an overgrowth of the cells lining the ducts of glands that resembles a papilla or nipple-like nodule/tumor. PB tumors develop in the apocrine glands of the breast. PB is also termed juvenile papillomatosis because of its frequent occurrence in younger women and Swiss cheese disease because of its microscopic appearance. Rarely, PB has also been diagnosed in very young, adolescent, and adult males.
Papillary carcinomas of the breast (PCB), also termed malignant papillary carcinomas of the breast, are rare forms of the breast cancers. The World Health Organization (2019) classified papillary neoplasms of the breast into 5 types: intraductal papilloma, papillary ductal carcinoma in situ (PDCIS), encapsulated papillary carcinoma (EPC), solid-papillary carcinoma (SPC), and invasive papillary carcinoma (IPC). The latter four carcinomas are considered here; intraductal papilloma is a benign neoplasm. The World Health Organization regarded solid papillary carcinoma as having two subtypes: in situ and invasive SPC.