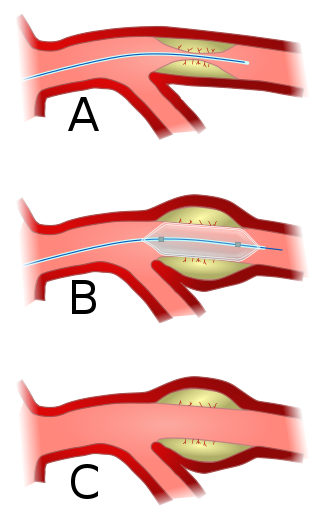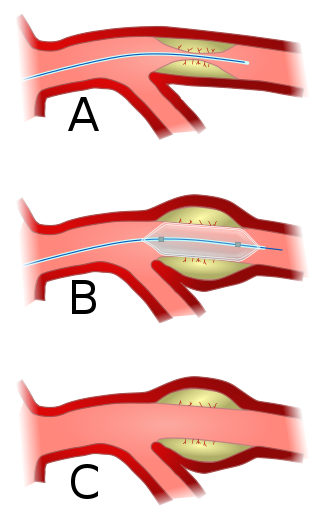
Angioplasty, also known as balloon angioplasty and percutaneous transluminal angioplasty (PTA), is a minimally invasive endovascular procedure used to widen narrowed or obstructed arteries or veins, typically to treat arterial atherosclerosis.

A coronary catheterization is a minimally invasive procedure to access the coronary circulation and blood filled chambers of the heart using a catheter. It is performed for both diagnostic and interventional (treatment) purposes.

dextro-Transposition of the great arteries is a potentially life-threatening birth defect in the large arteries of the heart. The primary arteries are transposed.

Mitral stenosis is a valvular heart disease characterized by the narrowing of the opening of the mitral valve of the heart. It is almost always caused by rheumatic valvular heart disease. Normally, the mitral valve is about 5 cm2 during diastole. Any decrease in area below 2 cm2 causes mitral stenosis. Early diagnosis of mitral stenosis in pregnancy is very important as the heart cannot tolerate increased cardiac output demand as in the case of exercise and pregnancy. Atrial fibrillation is a common complication of resulting left atrial enlargement, which can lead to systemic thromboembolic complications such as stroke.

Restenosis is the recurrence of stenosis, a narrowing of a blood vessel, leading to restricted blood flow. Restenosis usually pertains to an artery or other large blood vessel that has become narrowed, received treatment to clear the blockage, and subsequently become re-narrowed. This is usually restenosis of an artery, or other blood vessel, or possibly a vessel within an organ.

Stenosis is the abnormal narrowing of a blood vessel or other tubular organ or structure such as foramina and canals. It is also sometimes called a stricture.

Interventional cardiology is a branch of cardiology that deals specifically with the catheter based treatment of structural heart diseases. Andreas Gruentzig is considered the father of interventional cardiology after the development of angioplasty by interventional radiologist Charles Dotter.

Cardiac catheterization is the insertion of a catheter into a chamber or vessel of the heart. This is done both for diagnostic and interventional purposes.

Renovascular hypertension is a condition in which high blood pressure is caused by the kidneys' hormonal response to narrowing of the arteries supplying the kidneys. When functioning properly this hormonal axis regulates blood pressure. Due to low local blood flow, the kidneys mistakenly increase blood pressure of the entire circulatory system. It is a form of secondary hypertension - a form of hypertension whose cause is identifiable.

Pulmonary valve stenosis (PVS) is a heart valve disorder. Blood going from the heart to the lungs goes through the pulmonary valve, whose purpose is to prevent blood from flowing back to the heart. In pulmonary valve stenosis this opening is too narrow, leading to a reduction of flow of blood to the lungs.
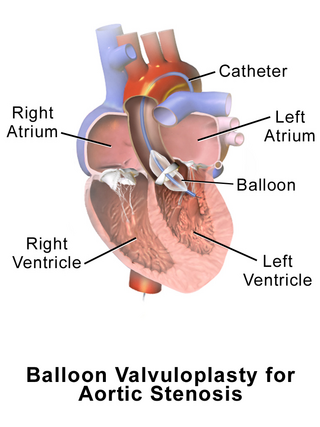
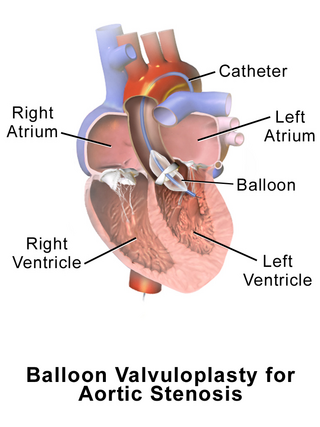
Aortic valvuloplasty, also known as balloon aortic valvuloplasty (BAV), is a procedure used to improve blood flow through the aortic valve in conditions that cause aortic stenosis, or narrowing of the aortic valve. It can be performed in various patient populations including fetuses, newborns, children, adults, and pregnant women. The procedure involves using a balloon catheter to dilate the narrowed aortic valve by inflating the balloon.

Carotid artery stenting is an endovascular procedure where a stent is deployed within the lumen of the carotid artery to treat narrowing of the carotid artery and decrease the risk of stroke. It is used to treat narrowing of the carotid artery in high-risk patients, when carotid endarterectomy is considered too risky.

Lutembacher's syndrome is a very rare form of congenital heart disease that affects one of the chambers of the heart as well as a valve. It is commonly known as both congenital atrial septal defect (ASD) and acquired mitral stenosis (MS). Congenital atrial septal defect refers to a hole being in the septum or wall that separates the two atria; this condition is usually seen in fetuses and infants. Mitral stenosis refers to mitral valve leaflets sticking to each other making the opening for blood to pass from the atrium to the ventricles very small. With the valve being so small, blood has difficulty passing from the left atrium into the left ventricle. Septal defects that may occur with Lutembacher's syndrome include: Ostium primum atrial septal defect or ostium secundum which is more prevalent.

A coronary stent is a tube-shaped device placed in the coronary arteries that supply blood to the heart, to keep the arteries open in patients suffering from coronary heart disease. The vast majority of stents used in modern interventional cardiology are drug-eluting stents (DES). They are used in a medical procedure called percutaneous coronary intervention (PCI). Coronary stents are divided into two broad types: drug-eluting and bare metal stents. As of 2023, drug-eluting stents were used in more than 90% of all PCI procedures. Stents reduce angina and have been shown to improve survival and decrease adverse events after a patient has suffered a heart attack—medically termed an acute myocardial infarction.
The following outline is provided as an overview of and topical guide to cardiology, the branch of medicine dealing with disorders of the human heart. The field includes medical diagnosis and treatment of congenital heart defects, coronary artery disease, heart failure, valvular heart disease and electrophysiology. Physicians who specialize in cardiology are called cardiologists.

Congenital stenosis of vena cava is a congenital anomaly in which the superior vena cava or inferior vena cava has an aberrant interruption or coarctation.

Arterial embolism is a sudden interruption of blood flow to an organ or body part due to an embolus adhering to the wall of an artery blocking the flow of blood, the major type of embolus being a blood clot (thromboembolism). Sometimes, pulmonary embolism is classified as arterial embolism as well, in the sense that the clot follows the pulmonary artery carrying deoxygenated blood away from the heart. However, pulmonary embolism is generally classified as a form of venous embolism, because the embolus forms in veins. Arterial embolism is the major cause of infarction.
Pulmonary Artery Banding (PAB) was introduced by Muller and Dammann in 1951 as a surgical technique to reduce excessive pulmonary blood flow in infants suffering from congenital heart defects. PAB is a palliative operation as it does not correct the problems, but attempts to improve abnormal heart function, relieve symptoms and reduce high pressure in the lungs. The use of PAB has decreased over the years due to advancements in definitive surgical repairs, however PAB still has widespread clinical use. PAB is commonly used in patients when definitive surgical repair is not feasible.

A hybrid cardiac surgical procedure in a narrow sense is defined as a procedure that combines a conventional, more invasive surgical part with an interventional part, using some sort of catheter-based procedure guided by fluoroscopy imaging in a hybrid operating room (OR) without interruption. The hybrid technique has a reduced risk of surgical complications and has shown decreased recovery time. It can be used to treat numerous heart diseases and conditions and with the increasing complexity of each case, the hybrid surgical technique is becoming more common.

Balloon pulmonary angioplasty (BPA) is an emerging minimally invasive procedure to treat chronic thromboembolic pulmonary hypertension (CTEPH) in people who are not suitable for pulmonary thromboendarterectomy (PTE) or still have residual pulmonary hypertension and areas of narrowing in the pulmonary arterial tree following previous PTE.