Related Research Articles
Non-Hodgkin lymphoma (NHL), also known as non-Hodgkin's lymphoma, is a group of blood cancers that includes all types of lymphomas except Hodgkin lymphomas. Symptoms include enlarged lymph nodes, fever, night sweats, weight loss, and tiredness. Other symptoms may include bone pain, chest pain, or itchiness. Some forms are slow-growing while others are fast-growing. Unlike Hodgkin lymphoma, which spreads contiguously, NHL is largely a systemic illness.

Lymphoma is a group of blood and lymph tumors that develop from lymphocytes. The name typically refers to just the cancerous versions rather than all such tumours. Signs and symptoms may include enlarged lymph nodes, fever, drenching sweats, unintended weight loss, itching, and constantly feeling tired. The enlarged lymph nodes are usually painless. The sweats are most common at night.

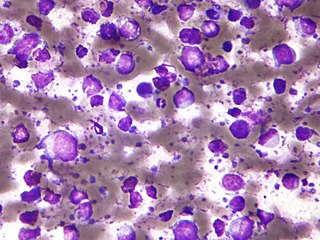
Burkitt lymphoma is a cancer of the lymphatic system, particularly B lymphocytes found in the germinal center. It is named after Denis Parsons Burkitt, the Irish surgeon who first described the disease in 1958 while working in equatorial Africa. It is a highly aggressive form of cancer which often, but not always, manifests after a person develops acquired immunodeficiency from infection with Epstein-Barr Virus or Human Immunodeficiency Virus (HIV).

Tumors of the hematopoietic and lymphoid tissues or tumours of the haematopoietic and lymphoid tissues are tumors that affect the blood, bone marrow, lymph, and lymphatic system. Because these tissues are all intimately connected through both the circulatory system and the immune system, a disease affecting one will often affect the others as well, making aplasia, myeloproliferation and lymphoproliferation closely related and often overlapping problems. While uncommon in solid tumors, chromosomal translocations are a common cause of these diseases. This commonly leads to a different approach in diagnosis and treatment of hematological malignancies. Hematological malignancies are malignant neoplasms ("cancer"), and they are generally treated by specialists in hematology and/or oncology. In some centers "hematology/oncology" is a single subspecialty of internal medicine while in others they are considered separate divisions. Not all hematological disorders are malignant ("cancerous"); these other blood conditions may also be managed by a hematologist.
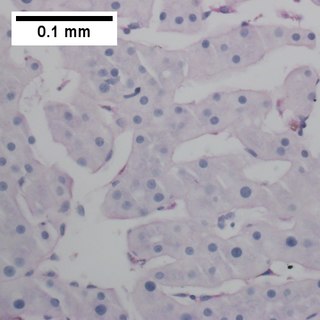
Primary effusion lymphoma (PEL) is classified as a diffuse large B cell lymphoma. It is a rare malignancy of plasmablastic cells that occurs in individuals that are infected with the Kaposi's sarcoma-associated herpesvirus. Plasmablasts are immature plasma cells, i.e. lymphocytes of the B-cell type that have differentiated into plasmablasts but because of their malignant nature do not differentiate into mature plasma cells but rather proliferate excessively and thereby cause life-threatening disease. In PEL, the proliferating plasmablastoid cells commonly accumulate within body cavities to produce effusions, primarily in the pleural, pericardial, or peritoneal cavities, without forming a contiguous tumor mass. In rare cases of these cavitary forms of PEL, the effusions develop in joints, the epidural space surrounding the brain and spinal cord, and underneath the capsule which forms around breast implants. Less frequently, individuals present with extracavitary primary effusion lymphomas, i.e., solid tumor masses not accompanied by effusions. The extracavitary tumors may develop in lymph nodes, bone, bone marrow, the gastrointestinal tract, skin, spleen, liver, lungs, central nervous system, testes, paranasal sinuses, muscle, and, rarely, inside the vasculature and sinuses of lymph nodes. As their disease progresses, however, individuals with the classical effusion-form of PEL may develop extracavitary tumors and individuals with extracavitary PEL may develop cavitary effusions.

T cell lymphoma is a rare form of cancerous lymphoma affecting T cells. Lymphoma arises mainly from the uncontrolled proliferation of T cells and can become cancerous.

Primary central nervous system lymphoma (PCNSL), also termed primary diffuse large B-cell lymphoma of the central nervous system (DLBCL-CNS), is a primary intracranial tumor appearing mostly in patients with severe immunodeficiency. It is a subtype and one of the most aggressive of the diffuse large B-cell lymphomas.
The B-cell lymphomas are types of lymphoma affecting B cells. Lymphomas are "blood cancers" in the lymph nodes. They develop more frequently in older adults and in immunocompromised individuals.
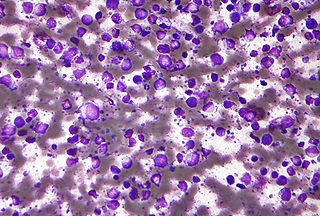
Diffuse large B-cell lymphoma (DLBCL) is a cancer of B cells, a type of lymphocyte that is responsible for producing antibodies. It is the most common form of non-Hodgkin lymphoma among adults, with an annual incidence of 7–8 cases per 100,000 people per year in the US and UK. This cancer occurs primarily in older individuals, with a median age of diagnosis at ~70 years, although it can occur in young adults and, in rare cases, children. DLBCL can arise in virtually any part of the body and, depending on various factors, is often a very aggressive malignancy. The first sign of this illness is typically the observation of a rapidly growing mass or tissue infiltration that is sometimes associated with systemic B symptoms, e.g. fever, weight loss, and night sweats.

Aggressive lymphoma, also known as high-grade lymphoma, is a group of fast growing non-Hodgkin lymphoma.

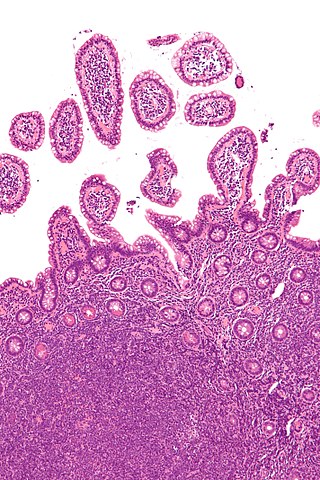
Marginal zone lymphomas, also known as marginal zone B-cell lymphomas (MZLs), are a heterogeneous group of lymphomas that derive from the malignant transformation of marginal zone B-cells. Marginal zone B cells are innate lymphoid cells that normally function by rapidly mounting IgM antibody immune responses to antigens such as those presented by infectious agents and damaged tissues. They are lymphocytes of the B-cell line that originate and mature in secondary lymphoid follicles and then move to the marginal zones of mucosa-associated lymphoid tissue (MALT), the spleen, or lymph nodes. Mucosa-associated lymphoid tissue is a diffuse system of small concentrations of lymphoid tissue found in various submucosal membrane sites of the body such as the gastrointestinal tract, mouth, nasal cavity, pharynx, thyroid gland, breast, lung, salivary glands, eye, skin and the human spleen.

The stages of HIV infection are acute infection, latency, and AIDS. Acute infection lasts for several weeks and may include symptoms such as fever, swollen lymph nodes, inflammation of the throat, rash, muscle pain, malaise, and mouth and esophageal sores. The latency stage involves few or no symptoms and can last anywhere from two weeks to twenty years or more, depending on the individual. AIDS, the final stage of HIV infection, is defined by low CD4+ T cell counts, various opportunistic infections, cancers, and other conditions.

Plasmablastic lymphoma (PBL) is a type of large B-cell lymphoma recognized by the World Health Organization (WHO) in 2017 as belonging to a subgroup of lymphomas termed lymphoid neoplasms with plasmablastic differentiation. The other lymphoid neoplasms within this subgroup are: plasmablastic plasma cell lymphoma ; primary effusion lymphoma that is Kaposi's sarcoma-associated herpesvirus positive or Kaposi's sarcoma-associated Herpesvirus negative; anaplastic lymphoma kinase-positive large B-cell lymphoma; and human herpesvirus 8-positive diffuse large B-cell lymphoma, not otherwise specified. All of these lymphomas are malignancies of plasmablasts, i.e. B-cells that have differentiated into plasmablasts but because of their malignant nature: fail to differentiate further into mature plasma cells; proliferate excessively; and accumulate in and injure various tissues and organs.
Large B-cell lymphoma arising in HHV8-associated multicentric Castleman's disease is a type of large B-cell lymphoma, recognized in the WHO 2008 classification. It is sometimes called the plasmablastic form of multicentric Castleman disease. It has sometimes been confused with plasmablastic lymphoma in the literature, although that is a dissimilar specific entity. It has variable CD20 expression and unmutated immunoglobulin variable region genes.

Human herpesvirus 8 associated multicentric Castleman disease is a subtype of Castleman disease, a group of rare lymphoproliferative disorders characterized by lymph node enlargement, characteristic features on microscopic analysis of enlarged lymph node tissue, and a range of symptoms and clinical findings.

Idiopathic multicentric Castleman disease (iMCD) is a subtype of Castleman disease (also known as giant lymph node hyperplasia, lymphoid hamartoma, or angiofollicular lymph node hyperplasia), a group of lymphoproliferative disorders characterized by lymph node enlargement, characteristic features on microscopic analysis of enlarged lymph node tissue, and a range of symptoms and clinical findings.
Epstein–Barr virus–associated lymphoproliferative diseases are a group of disorders in which one or more types of lymphoid cells, i.e. B cells, T cells, NK cells, and histiocytic-dendritic cells, are infected with the Epstein–Barr virus (EBV). This causes the infected cells to divide excessively, and is associated with the development of various non-cancerous, pre-cancerous, and cancerous lymphoproliferative disorders (LPDs). These LPDs include the well-known disorder occurring during the initial infection with the EBV, infectious mononucleosis, and the large number of subsequent disorders that may occur thereafter. The virus is usually involved in the development and/or progression of these LPDs although in some cases it may be an "innocent" bystander, i.e. present in, but not contributing to, the disease.

Indolent lymphoma, also known as low-grade lymphoma, is a group of slow-growing non-Hodgkin lymphomas (NHLs). Because they spread slowly, they tend to have fewer signs and symptoms when first diagnosed and may not require immediate treatment. Symptoms can include swollen but painless lymph nodes, unexplained fever, and unintended weight loss.
Mature T-cell lymphoma, also called peripheral T-cell lymphoma, is a group of rare, aggressive lymphomas that develop from mature white blood cells and originate from lymphoid tissues outside of the bone marrow. Mature T-cell lymphoma is under the category of non-Hodgkin lymphoma. Mature T-cell lymphomas account for 10% to 15% of all lymphomas and is more common in Asia than in Europe and America. Its common subtypes include angioimmunoblastic T-cell lymphoma, anaplastic large cell lymphoma and peripheral T-cell lymphoma not otherwise specified. While different subtypes have variable symptoms, common symptoms include enlarged painless lymph nodes, fever, weight loss, rash and night sweats.
Central Nervous System Prophylaxis, or CNS prophylaxis, is a type of chemotherapy for patients at risk of cancer metastasis into the central nervous system (CNS). Prophylaxis originated from the Greek word “phulaxis”, meaning the act of guarding. CNS prophylaxis refers to preventative measures that kill cancer cells potentially in the intrathecal space and the organs of the central nervous system.
References
- ↑ Besson C, Goubar A, Gabarre J, et al. (October 2001). "Changes in AIDS-related lymphoma since the era of highly active antiretroviral therapy". Blood. 98 (8): 2339–44. doi: 10.1182/blood.V98.8.2339 . PMID 11588028.
- ↑ Rigolet A, Bossi P, Caumes E, et al. (September 2001). "Caractéristiques épidémiologiques et évolution de l'incidence des lymphomes cérébraux primitifs observés chez 80 patients infectés par le VIH entre 1983 et 1999" [Epidemiological features and incidence trends of primary cerebral lymphomas observed in 80 HIV-infected patients from 1983 to 1999]. Pathologie-biologie (in French). 49 (7): 572–5. doi:10.1016/S0369-8114(01)00206-1. PMID 11642021.
- ↑ "AIDS-Related Lymphoma Treatment (PDQ®) - National Cancer Institute". Cancer.gov. 2012-05-18. Retrieved 2012-05-30.
- ↑ "UpToDate". UpToDate. Retrieved February 10, 2024.
- ↑ Heise, Walter (2010). "GI-lymphomas in immunosuppressed patients (organ transplantation; HIV)". Best Practice & Research Clinical Gastroenterology. 24 (1). Elsevier BV: 57–69. doi:10.1016/j.bpg.2010.01.001. ISSN 1521-6918. PMID 20206109.
- ↑ Noy, Ariela (2020). "HIV Lymphoma and Burkitts Lymphoma". The Cancer Journal. 26 (3). Ovid Technologies (Wolters Kluwer Health): 260–268. doi:10.1097/ppo.0000000000000448. ISSN 1540-336X. PMC 9302611 . PMID 32496459.
- ↑ Abellán-Martínez, Javier; Guerra-Vales, Juan-Manuel; Fernández-Cotarelo, María-José; González-Alegre, María-Teresa (2009). "Evolution of the incidence and aetiology of fever of unknown origin (FUO), and survival in HIV-infected patients after HAART (Highly Active Antiretroviral Therapy)". European Journal of Internal Medicine. 20 (5). Elsevier BV: 474–477. doi:10.1016/j.ejim.2009.01.004. ISSN 0953-6205. PMID 19712847.
- ↑ Brunnberg, Uta; Hentrich, Marcus; Hoffmann, Christian; Wolf, Timo; Hübel, Kai (2017). "HIV-Associated Malignant Lymphoma". Oncology Research and Treatment. 40 (3). S. Karger AG: 82–87. doi:10.1159/000456036. ISSN 2296-5270. PMID 28253516.
- ↑ Xie, Yi; Pittaluga, Stefania; Jaffe, Elaine S. (2015). "The Histological Classification of Diffuse Large B-cell Lymphomas". Seminars in Hematology. 52 (2). Elsevier BV: 57–66. doi:10.1053/j.seminhematol.2015.01.006. ISSN 0037-1963. PMC 4374126 . PMID 25805585.
- 1 2 Re, Alessandro; Cattaneo, Chiara; Rossi, Giuseppe (January 1, 2019). "HIV and Lymphoma: From Epidemiology to Clinical Management". Mediterranean Journal of Hematology and Infectious Diseases. 11 (1). Institute of Hematology, Catholic University: e2019004. doi:10.4084/mjhid.2019.004. ISSN 2035-3006. PMC 6328036 . PMID 30671210.
- ↑ Magangane, Pumza S.; Mohamed, Zainab; Naidoo, Richard (February 24, 2020). "Diffuse large B-cell lymphoma in a high human immunodeficiency virus (HIV) prevalence, low-resource setting". South African Journal of Oncology. 4. AOSIS. doi: 10.4102/sajo.v4i0.104 . ISSN 2518-8704.
- ↑ Wu, Dedong; Chen, Chen; Zhang, Mingzhi; Li, Zhaoming; Wang, Suqian; Shi, Jijing; Zhang, Yu; Yao, Dingzhu; Hu, Shuang (March 29, 2019). "The clinical features and prognosis of 100 AIDS-related lymphoma cases". Scientific Reports. 9 (1). Springer Science and Business Media LLC: 5381. Bibcode:2019NatSR...9.5381W. doi:10.1038/s41598-019-41869-9. ISSN 2045-2322. PMC 6441082 . PMID 30926889.
- 1 2 Meister, Anne; Hentrich, Marcus; Wyen, Christoph; Hübel, Kai (May 22, 2018). "Malignant lymphoma in the <scp>HIV</scp>-positive patient". European Journal of Haematology. 101 (1). Wiley: 119–126. doi:10.1111/ejh.13082. ISSN 0902-4441. PMID 29663523.
- 1 2 3 4 5 6 7 8 9 Berhan, Ayenew; Bayleyegn, Biruk; Getaneh, Zegeye (2022). "HIV/AIDS Associated Lymphoma: Review". Blood and Lymphatic Cancer: Targets and Therapy. 12. Informa UK Limited: 31–45. doi: 10.2147/blctt.s361320 . ISSN 1179-9889. PMC 9063794 . PMID 35517869.
- ↑ Shah, Hina J.; Keraliya, Abhishek R.; Jagannathan, Jyothi P.; Tirumani, Sree Harsha; Lele, Vikram R.; DiPiro, Pamela J. (2017). "Diffuse Large B-Cell Lymphoma in the Era of Precision Oncology: How Imaging Is Helpful". Korean Journal of Radiology. 18 (1). The Korean Society of Radiology: 54–70. doi:10.3348/kjr.2017.18.1.54. ISSN 1229-6929. PMC 5240489 . PMID 28096718.
- ↑ Pinisetti, S.; Nalabolu, G. R.; Uvr, C.; Tadi, D. P. (2013). "HIV Associated Intra–oral Burkitt's Lymphoma: A Case Report". Journal of Clinical and Diagnostic Research. 7 (12). JCDR Research and Publications: 3088–3089. doi:10.7860/jcdr/2013/6715.3862. ISSN 2249-782X. PMC 3919292 . PMID 24551737.
- 1 2 Ansorge, Rick (November 1, 2021). "Burkitt Lymphoma: Diagnosis, Prognosis, Symptoms, and Treatments". WebMD. Retrieved February 11, 2024.
- ↑ Dozzo, Massimo; Carobolante, Francesca; Donisi, Pietro Maria; Scattolin, Annamaria; Maino, Elena; Sancetta, Rosaria; Viero, Piera; Bassan, Renato (2016). "Burkitt lymphoma in adolescents and young adults: management challenges". Adolescent Health, Medicine and Therapeutics. 8. Informa UK Limited: 11–29. doi: 10.2147/ahmt.s94170 . ISSN 1179-318X. PMC 5207020 . PMID 28096698.
- ↑ Grommes, Christian; DeAngelis, Lisa M. (July 20, 2017). "Primary CNS Lymphoma". Journal of Clinical Oncology. 35 (21). American Society of Clinical Oncology (ASCO): 2410–2418. doi:10.1200/jco.2017.72.7602. ISSN 0732-183X. PMC 5516483 . PMID 28640701.
- ↑ Dunleavy, Kieron; Wilson, Wyndham H. (April 5, 2012). "How I treat HIV-associated lymphoma". Blood. 119 (14). American Society of Hematology: 3245–3255. doi:10.1182/blood-2011-08-373738. ISSN 0006-4971. PMC 3321851 . PMID 22337719.
- ↑ Zhao, Hui; Ma, Miao; Zhang, Limin; Zheng, Guanghui; Lv, Hong; Liu, Jie; Li, Xiao; Song, Bei; Zhang, Guojun (May 7, 2019). "Diagnosis of central nervous system lymphoma via cerebrospinal fluid cytology: a case report". BMC Neurology. 19 (1). Springer Science and Business Media LLC: 90. doi: 10.1186/s12883-019-1317-3 . ISSN 1471-2377. PMC 6505083 . PMID 31064334.
- ↑ Jarrett, Ruth F (December 17, 2005). "Viruses and lymphoma/leukaemia". The Journal of Pathology. 208 (2). Wiley: 176–186. doi:10.1002/path.1905. ISSN 0022-3417. PMID 16362996.
- ↑ Antar, A; El Hajj, H; Jabbour, M; Khalifeh, I; EL-Merhi, F; Mahfouz, R; Bazarbachi, A (March 7, 2014). "Primary effusion lymphoma in an elderly patient effectively treated by lenalidomide: case report and review of literature". Blood Cancer Journal. 4 (3). Springer Science and Business Media LLC: e190. doi:10.1038/bcj.2014.6. ISSN 2044-5385. PMC 3972705 . PMID 24608734.
- ↑ Narkhede, Mayur; Arora, Shagun; Ujjani, Chaitra (2018). "Primary effusion lymphoma: current perspectives". OncoTargets and Therapy. 11. Informa UK Limited: 3747–3754. doi: 10.2147/ott.s167392 . ISSN 1178-6930. PMC 6029609 . PMID 29988764.
- ↑ Castillo, Jorge J.; Bibas, Michele; Miranda, Roberto N. (April 9, 2015). "The biology and treatment of plasmablastic lymphoma". Blood. 125 (15). American Society of Hematology: 2323–2330. doi:10.1182/blood-2014-10-567479. ISSN 0006-4971. PMID 25636338.
- ↑ Castillo, Jorge; Reagan, John (2011). "Plasmablastic Lymphoma: A Systematic Review". Scientific World Journal. 11: 687–96. doi: 10.1100/tsw.2011.59 . PMC 5720057 . PMID 21442146.
- ↑ Broccoli, Alessandro; Nanni, Laura; Stefoni, Vittorio; Agostinelli, Claudio; Argnani, Lisa; Cavo, Michele; Zinzani, Pier Luigi (June 8, 2018). "A patient with plasmablastic lymphoma achieving long-term complete remission after thalidomide-dexamethasone induction and double autologous stem cell transplantation: a case report". BMC Cancer. 18 (1). Springer Science and Business Media LLC: 645. doi: 10.1186/s12885-018-4561-9 . ISSN 1471-2407. PMC 5992724 . PMID 29879938.
- ↑ Ul-Haq, Ikram; Dalla Pria, Alessia; Suardi, Elisa; Pinato, David J.; Froeling, Fieke; Forni, John; Randell, Paul; Bower, Mark (March 13, 2018). "Blood Epstein–Barr virus DNA does not predict outcome in advanced HIV-associated Hodgkin lymphoma". Medical Oncology. 35 (4). Springer Science and Business Media LLC: 53. doi:10.1007/s12032-018-1099-2. hdl: 10044/1/58296 . ISSN 1357-0560. PMC 5849636 . PMID 29536181.
- ↑ Grogg, K L; Miller, R F; Dogan, A (December 20, 2006). "HIV infection and lymphoma". Journal of Clinical Pathology. 60 (12). BMJ: 1365–1372. doi:10.1136/jcp.2007.051953. ISSN 0021-9746. PMC 2095580 . PMID 18042692.
- ↑ Yarchoan, Robert; Uldrick, Thomas S. (March 15, 2018). "HIV-Associated Cancers and Related Diseases". New England Journal of Medicine. 378 (11). Massachusetts Medical Society: 1029–1041. doi:10.1056/nejmra1615896. ISSN 0028-4793. PMC 6890231 . PMID 29539283.