Platelets, also called thrombocytes, are a component of blood whose function is to react to bleeding from blood vessel injury by clumping, thereby initiating a blood clot. Platelets have no cell nucleus; they are fragments of cytoplasm that are derived from the megakaryocytes of the bone marrow or lung, which then enter the circulation. Circulating inactivated platelets are biconvex discoid (lens-shaped) structures, 2–3 µm in greatest diameter. Activated platelets have cell membrane projections covering their surface. Platelets are found only in mammals, whereas in other vertebrates, thrombocytes circulate as intact mononuclear cells.

Coagulation, also known as clotting, is the process by which blood changes from a liquid to a gel, forming a blood clot. It potentially results in hemostasis, the cessation of blood loss from a damaged vessel, followed by repair. The mechanism of coagulation involves activation, adhesion and aggregation of platelets, as well as deposition and maturation of fibrin.

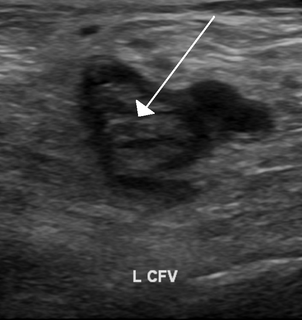
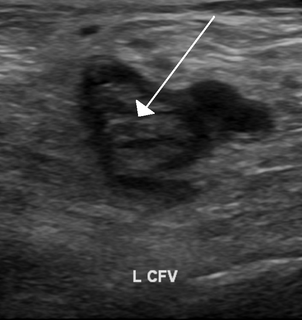
Disseminated intravascular coagulation (DIC) is a condition in which blood clots form throughout the body, blocking small blood vessels. Symptoms may include chest pain, shortness of breath, leg pain, problems speaking, or problems moving parts of the body. As clotting factors and platelets are used up, bleeding may occur. This may include blood in the urine, blood in the stool, or bleeding into the skin. Complications may include organ failure.

Antiphospholipid syndrome, or antiphospholipid antibody syndrome, is an autoimmune, hypercoagulable state caused by antiphospholipid antibodies. APS provokes blood clots (thrombosis) in both arteries and veins as well as pregnancy-related complications such as miscarriage, stillbirth, preterm delivery, and severe preeclampsia. Although the exact etiology of APS is still not clear, genetics is believed to play a key role in the development of the disease. The diagnostic criteria require one clinical event and two positive blood test results spaced at least three months apart that detect lupus anticoagulant, anti-apolipoprotein antibodies, or anti-cardiolipin antibodies.

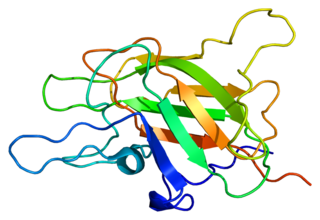
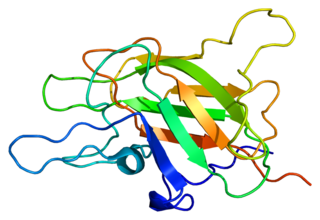
Fibrinogen is a glycoprotein complex, produced in the liver, that circulates in the blood of all vertebrates. During tissue and vascular injury, it is converted enzymatically by thrombin to fibrin and then to a fibrin-based blood clot. Fibrin clots function primarily to occlude blood vessels to stop bleeding. Fibrin also binds and reduces the activity of thrombin. This activity, sometimes referred to as antithrombin I, limits clotting. Fibrin also mediates blood platelet and endothelial cell spreading, tissue fibroblast proliferation, capillary tube formation, and angiogenesis and thereby promotes revascularization and wound healing.

Thrombin is a serine protease, an enzyme that, in humans, is encoded by the F2 gene. Prothrombin is proteolytically cleaved to form thrombin in the clotting process. Thrombin in turn acts as a serine protease that converts soluble fibrinogen into insoluble strands of fibrin, as well as catalyzing many other coagulation-related reactions.

Von Willebrand disease (VWD) is the most common hereditary blood-clotting disorder in humans. An acquired form can sometimes result from other medical conditions. It arises from a deficiency in the quality or quantity of von Willebrand factor (VWF), a multimeric protein that is required for platelet adhesion. It is known to affect several breeds of dogs as well as humans. The three forms of VWD are hereditary, acquired, and pseudo or platelet type. The three types of hereditary VWD are VWD type 1, VWD type 2, and VWD type 3. Type 2 contains various subtypes. Platelet type VWD is also an inherited condition.

The partial thromboplastin time (PTT), also known as the activated partial thromboplastin time, is a blood test that characterizes coagulation of the blood. A historical name for this measure is the kaolin-cephalin clotting time (KCCT), reflecting kaolin and cephalin as materials historically used in the test. Apart from detecting abnormalities in blood clotting, partial thromboplastin time is also used to monitor the treatment effect of heparin, a widely prescribed drug that reduces blood's tendency to clot.
Thrombophilia is an abnormality of blood coagulation that increases the risk of thrombosis. Such abnormalities can be identified in 50% of people who have an episode of thrombosis that was not provoked by other causes. A significant proportion of the population has a detectable thrombophilic abnormality, but most of these develop thrombosis only in the presence of an additional risk factor.
Factor V is a protein of the coagulation system, rarely referred to as proaccelerin or labile factor. In contrast to most other coagulation factors, it is not enzymatically active but functions as a cofactor. Deficiency leads to predisposition for hemorrhage, while some mutations predispose for thrombosis.

Factor XI or plasma thromboplastin antecedent is the zymogen form of factor XIa, one of the enzymes of the coagulation cascade. Like many other coagulation factors, it is a serine protease. In humans, Factor XI is encoded by the F11 gene.
Thromboelastography (TEG) is a method of testing the efficiency of blood coagulation. It is a test mainly used in surgery and anesthesiology, although increasingly used in resuscitations in Emergency Departments, intensive care units, and labor and delivery suites. More common tests of blood coagulation include prothrombin time (PT) and partial thromboplastin time (aPTT) which measure coagulation factor function, but TEG also can assess platelet function, clot strength, and fibrinolysis which these other tests cannot.

Hypoprothrombinemia is a rare blood disorder in which a deficiency in immunoreactive prothrombin, produced in the liver, results in an impaired blood clotting reaction, leading to an increased physiological risk for spontaneous bleeding. This condition can be observed in the gastrointestinal system, cranial vault, and superficial integumentary system, affecting both the male and female population. Prothrombin is a critical protein that is involved in the process of hemostasis, as well as illustrating procoagulant activities. This condition is characterized as an autosomal recessive inheritance congenital coagulation disorder affecting 1 per 2,000,000 of the population, worldwide, but is also attributed as acquired.
Thromboplastin (TPL) or thrombokinase is a mixture of both phospholipids and tissue factor found in plasma aiding blood coagulation through catalyzing the conversion of prothrombin to thrombin. It is a complex enzyme that is found in brain, lung, and other tissues and especially in blood platelets and that functions in the conversion of prothrombin to thrombin in the clotting of blood.
The dysfibrinogenemias consist of three types of fibrinogen disorders in which a critical blood clotting factor, fibrinogen, circulates at normal levels but is dysfunctional. Congenital dysfibrinogenemia is an inherited disorder in which one of the parental genes produces an abnormal fibrinogen. This fibrinogen interferes with normal blood clotting and/or lysis of blood clots. The condition therefore may cause pathological bleeding and/or thrombosis. Acquired dysfibrinogenemia is a non-hereditary disorder in which fibrinogen is dysfunctional due to the presence of liver disease, autoimmune disease, a plasma cell dyscrasias, or certain cancers. It is associated primarily with pathological bleeding. Hereditary fibrinogen Aα-Chain amyloidosis is a sub-category of congenital dysfibrinogenemia in which the dysfunctional fibrinogen does not cause bleeding or thrombosis but rather gradually accumulates in, and disrupts the function of, the kidney.
Venom-induced consumption coagulopathy (VICC) is a medical condition caused by the effects of some snake and caterpillar venoms on the blood. Important coagulation factors are activated by the specific serine proteases in the venom and as they become exhausted, coagulopathy develops. Symptoms are consistent with uncontrolled bleeding. Diagnosis is made using blood tests that assess clotting ability along with recent history of envenomation. Treatment generally involves pressure dressing, confirmatory blood testing, and antivenom administration.
The fibrinolysis system is responsible for removing blood clots. Hyperfibrinolysis describes a situation with markedly enhanced fibrinolytic activity, resulting in increased, sometimes catastrophic bleeding. Hyperfibrinolysis can be caused by acquired or congenital reasons. Among the congenital conditions for hyperfibrinolysis, deficiency of alpha-2-antiplasmin or plasminogen activator inhibitor type 1 (PAI-1) are very rare. The affected individuals show a hemophilia-like bleeding phenotype. Acquired hyperfibrinolysis is found in liver disease, in patients with severe trauma, during major surgical procedures, and other conditions. A special situation with temporarily enhanced fibrinolysis is thrombolytic therapy with drugs which activate plasminogen, e.g. for use in acute ischemic events or in patients with stroke. In patients with severe trauma, hyperfibrinolysis is associated with poor outcome. Moreover, hyperfibrinolysis may be associated with blood brain barrier impairment, a plasmin-dependent effect due to an increased generation of bradykinin.
Thromboelastometry (TEM), previously named rotational thromboelastography (ROTEG) or rotational thromboelastometry (ROTEM), is an established viscoelastic method for hemostasis testing in whole blood. It is a modification of traditional thromboelastography (TEG). TEM investigates the interaction of coagulation factors, their inhibitors, anticoagulant drugs, blood cells, specifically platelets, during clotting and subsequent fibrinolysis. The rheological conditions mimic the sluggish flow of blood in veins. While traditional thromboelastography is a global assay for blood clotting disorders and drug effects, TEM is primarily used in combination with appropriate differential assays. They allow testing in the presence of therapeutic heparin concentrations and provide differential diagnostic information to support decisions in therapy. In numerous publications the validity of the method is shown. Application of TEM at the point of care (POC) or in emergency laboratories is getting more and more popular. TEM detects both hypo- and hyperfunctional stages of the clotting process and is probably the only reliable rapid test for the diagnosis of hyperfibrinolysis. In contrast to standard clotting tests, the fibrin stabilizing effect of factor XIII contributes to the result. The rapid availability of results helps to discriminate surgical bleeding from a true haemostasis disorder and improves the therapy with blood products, factor concentrates, anticoagulants and protamine, hemostyptic and antifibrinolytic drugs. Several reports confirm that application of TEM is cost effective by reducing the consumption of blood products.
Blood clotting tests are the tests used for diagnostics of the hemostasis system. Coagulometer is the medical laboratory analyzer used for testing of the hemostasis system. Modern coagulometers realize different methods of activation and observation of development of blood clots in blood or in blood plasma.
The overall hemostatic potential (OHP) test is a global coagulation assay which can be used to measure coagulation. The OHP assay measures total fibrin generation in the presence of thrombin or tissue factor and tissue plasminogen activator (t-PA). It generates a fibrin time curve through the use of optical density measurement. This curve represents the balance between fibrin formation induced by thrombin or tissue factor and fibrinolysis induced by t-PA. The assay provides three parameters: overall coagulation potential (OCP), overall hemostatic potential (OHP), and overall fibrinolytic potential (OFP). OHP is the main parameter, while OCP and OFP are supplementary parameters to assess coagulation and fibrinolysis. One further parameter, clot lysis time (CLT), can also be determined. The OHP assay measures the integrated effect of procoagulant, anticoagulant, and fibrinolytic factors.