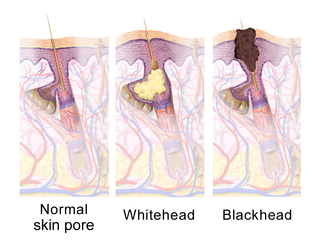
Acne, also known as acne vulgaris, is a long-term skin condition that occurs when dead skin cells and oil from the skin clog hair follicles. Typical features of the condition include blackheads or whiteheads, pimples, oily skin, and possible scarring. It primarily affects skin with a relatively high number of oil glands, including the face, upper part of the chest, and back. The resulting appearance can lead to lack of confidence, anxiety, reduced self-esteem, and, in extreme cases, depression or thoughts of suicide.

Isotretinoin, also known as 13-cis-retinoic acid and sold under the brand name Accutane among others, is a medication primarily used to treat severe acne. It is also used to prevent certain skin cancers, and in the treatment of other cancers. It is used to treat harlequin-type ichthyosis, a usually lethal skin disease, and lamellar ichthyosis. It is a retinoid, meaning it is related to vitamin A, and is found in small quantities naturally in the body. Its isomer, tretinoin, is also an acne drug.

Harlequin-type ichthyosis is a genetic disorder that results in thickened skin over nearly the entire body at birth. The skin forms large, diamond/trapezoid/rectangle-shaped plates that are separated by deep cracks. These affect the shape of the eyelids, nose, mouth, and ears and limit movement of the arms and legs. Restricted movement of the chest can lead to breathing difficulties. These plates fall off over several weeks. Other complications can include premature birth, infection, problems with body temperature, and dehydration. The condition is the most severe form of ichthyosis, a group of genetic disorders characterised by scaly skin.

Ichthyosis is a family of genetic skin disorders characterized by dry, thickened, scaly skin. The more than 20 types of ichthyosis range in severity of symptoms, outward appearance, underlying genetic cause and mode of inheritance. Ichthyosis comes from the Greek ἰχθύς ichthys, literally "fish", since dry, scaly skin is the defining feature of all forms of ichthyosis.

Epidermolytic ichthyosis (EI), also known as bullous epidermis ichthyosis (BEI), epidermolytic hyperkeratosis (EHK), bullous congenital ichthyosiform erythroderma (BCIE), bullous ichthyosiform erythroderma or bullous congenital ichthyosiform erythroderma Brocq, is a rare and severe form of ichthyosis that affects around 1 in 300,000 people. It is caused by a genetic mutation, and thus cannot be completely cured without some form of gene therapy.

Adapalene is a third-generation topical retinoid primarily used in the treatment of mild-moderate acne, and is also used off-label to treat keratosis pilaris as well as other skin conditions. Studies have found adapalene is as effective as other retinoids, while causing less irritation. It also has several advantages over other retinoids. The adapalene molecule is more stable compared to tretinoin and tazarotene, which leads to less concern for photodegradation. It is also chemically more stable compared to the other two retinoids, allowing it to be used in combination with benzoyl peroxide. Due to its effects on keratinocyte proliferation and differentiation, adapalene is superior to tretinoin for the treatment of comedonal acne and is often used as a first-line agent. The Swiss company Galderma sells adapalene under the brand-name product Differin.

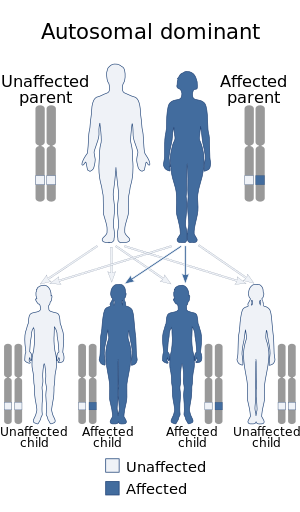
Darier's disease (DAR) is an inherited skin disorder that presents with multiple greasy, crusting, thick brown bumps that merge into patches. It is an autosomal dominant disorder discovered by French dermatologist Ferdinand-Jean Darier.

Hyperpigmentation is the darkening of an area of skin or nails caused by increased melanin.

Keratosis pilaris is a common, autosomal-dominant, genetic condition of the skin's hair follicles characterized by the appearance of possibly itchy, small, gooseflesh-like bumps, with varying degrees of reddening or inflammation. It most often appears on the outer sides of the upper arms, thighs, face, back, and buttocks; KP can also occur on the hands, and tops of legs, sides, or any body part except glabrous (hairless) skin. Often the lesions can appear on the face, which may be mistaken for acne or folliculitis.
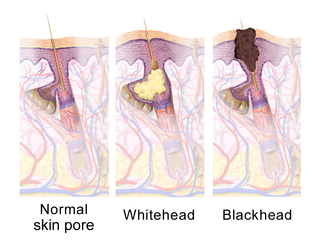
A comedo is a clogged hair follicle (pore) in the skin. Keratin combines with oil to block the follicle. A comedo can be open (blackhead) or closed by skin (whitehead) and occur with or without acne. The word "comedo" comes from the Latin comedere, meaning "to eat up", and was historically used to describe parasitic worms; in modern medical terminology, it is used to suggest the worm-like appearance of the expressed material.
Hailey–Hailey disease, or familial benign chronic pemphigus or familial benign pemphigus, was originally described by the Hailey brothers in 1939. It is a genetic disorder that causes blisters to form on the skin.
Acne cosmetica is a type of contact acneiform eruption caused by or aggravated by cosmetics. Signs and symptoms include a dense group of similar sized closed comedones and scattered small bumps, typically over the skin where the cosmetic has been applied. Flare-ups do not generally occur shortly before menstruation and open comedones are not common. There may be associated perioral dermatitis.

Genodermatosis is a hereditary skin disease with three inherited modes including single gene inheritance, multiple gene inheritance and chromosome inheritance. There are many different types of genodermatosis, the prevalence of genodermatosis ranges from 1 per 6000 people to 1 per 500,000 people. Genodermatosis has influence on the texture, color and structure of skin cuticle and connective tissue, specific lesion site and clinical manifestations on the body vary depending on the type. In the spite of the variety and complexity of genodermatosis, there are still some common methods that can help people diagnose. After diagnosis, different types of genodermatosis require different levels of therapy including interventions, nursing interventions and treatments. Among that, research of therapy for some new, complex and rare types are still in the developing stage. The impact of genodermatosis not only can be seen in body but also can be seen in all aspects of patients' life, including but not limited to psychological, family life, economic conditions and social activities. Accordingly, the patients need treatment, support and help in these areas.

Steatocystoma multiplex, is a benign, autosomal dominant congenital condition resulting in multiple cysts on a person's body. Steatocystoma simplex is the solitary counterpart to steatocystoma multiplex.

Ichthyosis bullosa of Siemens is a type of familial, autosomal dominant ichthyosis, a rare skin disorder. It is also known as bullous congenital ichthyosiform erythroderma of Siemens or ichthyosis exfoliativa. It is a genetic disorder with no known cure which is estimated to affect about 1 in 500,000 people.

Neonatal acne, also known as acne neonatorum, is an acneiform eruption that occurs in newborns or infants within the first 4-6 weeks of life, and presents with open and closed comedones on the cheeks, chin and forehead.

PAPA syndrome is a rare genetic disorder characterised by its effects on skin and joints. The acronym PAPA stands for pyogenic arthritis, pyoderma gangrenosum and acne.

Eosinophilic cellulitis, also known as Wells' syndrome, is a skin disease that presents with painful, red, raised, and warm patches of skin. The rash comes on suddenly, lasts for a few weeks, and often repeatedly comes back. Scar formation does not typically occur.

A pimple or zit is a kind of comedo that results from excess sebum and dead skin cells getting trapped in the pores of the skin. In its aggravated state, it may evolve into a pustule or papules. Pimples can be treated by acne medications, antibiotics, and anti-inflammatories prescribed by a physician, or various over the counter remedies purchased at a pharmacy.
Infantile acne is a form of acneiform eruption that occurs in infants from 6 weeks to 1 year of age. Typical symptoms include inflammatory and noninflammatory lesions, papules and pustules most commonly present on the face. No cause of infantile acne has been established but it may be caused by increased sebaceous gland secretions due to elevated androgens, genetics and the fetal adrenal gland causing increased sebum production. Infantile acne can resolve by itself by age 1 or 2. However, treatment options include topical benzyl peroxide, topical retinoids and topical antibiotics in most cases.