Diseases of affluence, previously called diseases of rich people, is a term sometimes given to selected diseases and other health conditions which are commonly thought to be a result of increasing wealth in a society. Also referred to as the "Western disease" paradigm, these diseases are in contrast to "diseases of poverty", which largely result from and contribute to human impoverishment. These diseases of affluence have vastly increased in prevalence since the end of World War II.

India's population in 2021 as per World Bank is 1.39 billion. Being the world's most populous country and one of its fastest-growing economies, India experiences both challenges and opportunities in context of public health. India is a hub for pharmaceutical and biotechnology industries; world-class scientists, clinical trials and hospitals yet country faces daunting public health challenges like child undernutrition, high rates of neonatal and maternal mortality, growth in noncommunicable diseases, high rates of road traffic accidents and other health related issues.

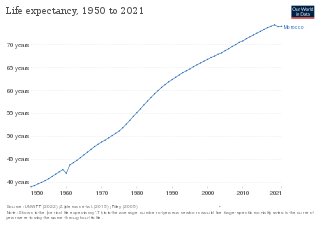
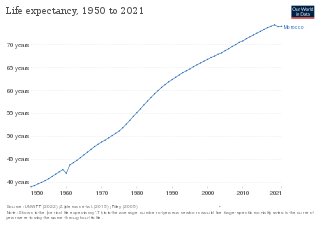
In demography and medical geography, epidemiological transition is a theory which "describes changing population patterns in terms of fertility, life expectancy, mortality, and leading causes of death." For example, a phase of development marked by a sudden increase in population growth rates brought by improved food security and innovations in public health and medicine, can be followed by a re-leveling of population growth due to subsequent declines in fertility rates. Such a transition can account for the replacement of infectious diseases by chronic diseases over time due to increased life span as a result of improved health care and disease prevention. This theory was originally posited by Abdel Omran in 1971.
Health in the United Kingdom refers to the overall health of the population of the United Kingdom. This includes overall trends such as life expectancy and mortality rates, mental health of the population and the suicide rate, smoking rates, alcohol consumption, prevalence of diseases within the population and obesity in the United Kingdom. Three of these – smoking rates, alcohol consumption and obesity – were above the OECD average in 2015.

Malaysia is classified by The World Bank as upper middle-income country and is attempting to achieve high-income status by 2020 and to move further up the value-added production chain by attracting investments in high technology, knowledge-based industries and services. Malaysia's HDI value for 2015 was recorded at 0.789 and HDI rank no 59 out of 188 countries and territories on the United Nations Development Programme's Human Development Index. In 2016, the population of Malaysia is 31 million; Total expenditure on health per capita is 1040; Total expenditure on health as % of GDP (2014) was 4.2. Gross national income (GNI) per capita was recorded at 24,620.

Pakistan is the fifth most populous country in the world with population approaching 225 million. It is a developing country struggling in many domains due to which the health system has suffered a lot. As a result of that, Pakistan is ranked 122nd out of 190 countries in the World Health Organization performance report.
Morocco became an independent country in 1956. At that time there were only 400 private practitioners and 300 public health physicians in the entire country. By 1992, the government had thoroughly improved their health care service and quality. Health care was made available to over 70% of the population. Programs and courses to teach health and hygiene have been introduced to inform parents and children on how to correctly care for their own and their families' health.

The Tajikistan health system is influenced by the former Soviet legacy. It is ranked as the poorest country within the WHO European region, including the lowest total health expenditure per capita. Tajikistan is ranked 129th as Human Development Index of 188 countries, with an Index of 0.627 in 2016. In 2016, the SDG Index value was 56. In Tajikistan health indicators such as infant and maternal mortality rates are among the highest of the former Soviet republics. In the post-Soviet era, life expectancy has decreased because of poor nutrition, polluted water supplies, and increased incidence of cholera, malaria, tuberculosis, and typhoid. Because the health care system has deteriorated badly and receives insufficient funding and because sanitation and water supply systems are in declining condition, Tajikistan has a high risk of epidemic disease.

Thailand has had "a long and successful history of health development," according to the World Health Organization. Life expectancy is averaged at eighty years. Non-communicable diseases form the major burden of morbidity and mortality, while infectious diseases including malaria and tuberculosis, as well as traffic accidents, are also important public health issues.
Chronic, non-communicable diseases account for an estimated 80% of total deaths and 70% of disability-adjusted life years (DALYs) lost in China. Cardiovascular diseases, chronic respiratory disease, and cancer are the leading causes of both death and of the burden of disease, and exposure to risk factors is high: more than 300 million men smoke cigarettes and 160 million adults are hypertensive, most of whom are not being treated. An obesity epidemic is imminent, with more than 20% of children aged 7–17 years in big cities now overweight or obese. Rates of death from chronic disease in middle-aged people are higher in China than in some high-income countries.

The healthcare system in Turkey has improved in terms of health status especially after implementing the Health Transformation Program (HP) in 2003. "Health for All" was the slogan for this transformation, and HP aimed to provide and finance health care efficiently, effectively, and equitably. By covering most of the population, the General Health Insurance Scheme is financed by employers, employees, and government contributions through the Social Security Institution. Even though HP aimed to be equitable, after 18 years of implementation, there are still disparities between the regions in Turkey. These discrepancies can be seen in terms of infant mortality between rural and urban areas and different parts of the country, although these have been declining over the years. While the under-5 mortality rate in Western Marmara is 7.9, the under-5 mortality rate in Southeastern Asia is two times higher than Western Marmara, with the rate of 16.3 in 2021.

The major causes of deaths in Finland are cardiovascular diseases, malignant tumors, dementia and Alzheimer's disease, respiratory diseases, alcohol related diseases and accidental poisoning by alcohol. In 2010, the leading causes of death among men aged 15 to 64 were alcohol-related deaths, ischaemic heart disease, accident, suicides, lung cancer and cerebrovascular diseases. Among women the leading causes were breast cancer, alcohol-related deaths, accidents, suicides, ischemic heart disease and lung cancer.

Niger is a landlocked country located in West Africa and has Libya, Chad, Nigeria, Benin, Mali, Burkina Faso, and Algeria as its neighboring countries. Niger was French territory that got its independence in 1960 and its official language is French. Niger has an area of 1.267 million square kilometres, nevertheless, 80% of its land area spreads through the Sahara Desert.

In precolonial Ghana, infectious diseases were the main cause of morbidity and mortality. The modern history of health in Ghana was heavily influenced by international actors such as Christian missionaries, European colonists, the World Bank, and the International Monetary Fund. In addition, the democratic shift in Ghana spurred healthcare reforms in an attempt to address the presence of infectious and noncommunicable diseases eventually resulting in the formation of the National Health insurance Scheme in place today.
According to the World Bank income level classification, Portugal is considered a high income country. In 2022, Portugal registered a total of 10,270,873 inhabitants with a expected decrease of 9.8% to 9,261,313 by 2050. The World Health Organization (WHO) estimates that 12.3% of the population is between 0-14 years, 68.2% is estimated to be 15-64 years and 19.5% is expected to be 65+ years old.
Zambia is a landlocked country in Sub Saharan Africa which experiences a burden of both communicable and non-communicable diseases. In line with WHO agenda for equity in health, it has adopted the Universal Health Coverage agenda to mitigate the challenges faced within the health sector. The Ministry of Health (MOH) provides information pertaining to Zambian health. The main focus of the Ministry of Health has been provision of uninterrupted care with emphasis on health systems strengthening and services via the primary health care approach.
Health in Malta has seen improvements in recent years, with one of the highest life expectancies in Europe. Malta has a good overall quality of health and has seen rapid growth and improvement in key health indicators. Malta has seen significant development in the practice of mental health which has been supported by new infrastructure and increased government health spending. The introduction of health-focused government initiatives, particularly around nutrition, alcohol, smoking, and health will likely contribute to the further improvement of overall health nationwide.
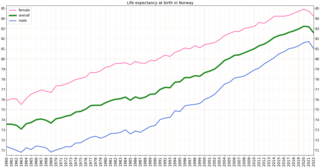
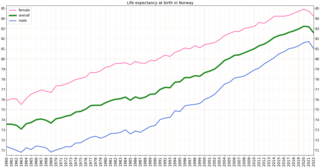
Health in Norway, with its early history of poverty and infectious diseases along with famines and epidemics, was poor for most of the population at least into the 1800s. The country eventually changed from a peasant society to an industrial one and established a public health system in 1860. Due to the high life expectancy at birth, the low under five mortality rate and the fertility rate in Norway, it is fair to say that the overall health status in the country is generally good.
Montenegro is a country with an area of 13,812 square kilometres and a population of 620,029, according to the 2011 census. The country is bordered by Croatia, the Adriatic Sea, Bosnia, Herzegovina, Serbia, Kosovo and Albania. The most common health issues faced are non-communicable diseases accounting for 95% of all deaths. This is followed by 4% of mortality due to injury, and 1% due to communicable, maternal, perinatal and nutritional conditions. Other health areas of interest are alcohol consumption, which is the most prevalent disease of addiction within Montenegro and smoking. Montenegro has one of the highest tobacco usage rates across Europe. Life expectancy for men is 74 years, and life expectancy for women is 79.
Within the Pacific, Tonga is recognised to have some of the highest overall health standards, implementing a combination of preventative and immediate strategies to curb rates of communicable disease, child mortality and overall life expectancy. The Tongan government aims to continue such levels of health through achieving their Millennium Development Goals (MDG) detailing their focus on improving their healthcare system within the areas of maternal and infant health as well as improve access to immunisation, safe water and sanitation.