Tropical medicine is an interdisciplinary branch of medicine that deals with health issues that occur uniquely, are more widespread, or are more difficult to control in tropical and subtropical regions.
In epidemiology, case fatality rate (CFR) – or sometimes more accurately case-fatality risk – is the proportion of people who have been diagnosed with a certain disease and end up dying of it. Unlike a disease's mortality rate, the CFR does not take into account the time period between disease onset and death. A CFR is generally expressed as a percentage. It is a measure of disease lethality, and thus may change with different treatments. CFRs are most often used for with discrete, limited-time courses, such as acute infections.

Joia Stapleton Mukherjee is an associate professor with the Division of Global Health Equity at the Brigham and Women's Hospital and the Department of Global Health and Social Medicine at Harvard Medical School. Since 2000, she has served as the Chief Medical Officer of Partners In Health, an international medical non-profit founded by Paul Farmer, Ophelia Dahl, and Jim Kim. She trained in Infectious Disease, Internal Medicine, and Pediatrics at the Massachusetts General Hospital and has an MPH from Harvard School of Public Health. Dr. Mukherjee has been involved in health care access and human rights issues since 1989, and she consults for the World Health Organization on the treatment of HIV and MDR-TB in developing countries. Her scholarly work focuses on the human rights aspect of HIV treatment and on the implementation of complex health interventions in resource-poor settings.

Mali, one of the world's poorest nations, is greatly affected by poverty, malnutrition, epidemics, and inadequate hygiene and sanitation. Mali's health and development indicators rank among the worst in the world, with little improvement over the last 20 years. Progress is impeded by Mali's poverty and by a lack of physicians. The 2012 conflict in northern Mali exacerbated difficulties in delivering health services to refugees living in the north. With a landlocked, agricultural-based economy, Mali is highly vulnerable to climate change. A catastrophic harvest in 2023 together with escalations in armed conflict have exacerbated food insecurity in Northern and Central Mali.
Morocco became an independent country in 1956. At that time there were only 400 private practitioners and 300 public health physicians in the entire country. By 1992, the government had thoroughly improved their health care service and quality. Health care was made available to over 70% of the population. Programs and courses to teach health and hygiene have been introduced to inform parents and children on how to correctly care for their own and their families' health.

Healthcare in Russia, or the Russian Federation, is provided by the state through the Federal Compulsory Medical Insurance Fund, and regulated through the Ministry of Health. The Constitution of the Russian Federation has provided all citizens the right to free healthcare since 1993. In 2008, 621,000 doctors and 1.3 million nurses were employed in Russian healthcare. The number of doctors per 10,000 people was 43.8, but only 12.1 in rural areas. The number of general practitioners as a share of the total number of doctors was 1.26 percent. There are about 9.3 beds per thousand population—nearly double the OECD average.

In the post-Soviet era, the quality of Uzbekistan’s health care has declined. Between 1992 and 2003, spending on health care and the ratio of hospital beds to population both decreased by nearly 50 percent, and Russian emigration in that decade deprived the health system of many practitioners. In 2004 Uzbekistan had 53 hospital beds per 10,000 population. Basic medical supplies such as disposable needles, anesthetics, and antibiotics are in very short supply. Although all citizens nominally are entitled to free health care, in the post-Soviet era bribery has become a common way to bypass the slow and limited service of the state system. In the early 2000s, policy has focused on improving primary health care facilities and cutting the cost of inpatient facilities. The state budget for 2006 allotted 11.1 percent to health expenditures, compared with 10.9 percent in 2005.
Health in Bhutan is one of the government's highest priorities in its scheme of development and modernization. Health and related issues are overseen by the Ministry of Health, itself represented on the executive Lhengye Zhungtshog (cabinet) by the Minister of Health. As a component of Gross National Happiness, affordable and accessible health care is central to the public policy of Bhutan.

A hospital is a healthcare institution providing patient treatment with specialized health science and auxiliary healthcare staff and medical equipment. The best-known type of hospital is the general hospital, which typically has an emergency department to treat urgent health problems ranging from fire and accident victims to a sudden illness. A district hospital typically is the major health care facility in its region, with many beds for intensive care and additional beds for patients who need long-term care.

In precolonial Ghana, infectious diseases were the main cause of morbidity and mortality. The modern history of health in Ghana was heavily influenced by international actors such as Christian missionaries, European colonists, the World Bank, and the International Monetary Fund. In addition, the democratic shift in Ghana spurred healthcare reforms in an attempt to address the presence of infectious and noncommunicable diseases eventually resulting in the formation of the National Health insurance Scheme in place today.
Healthcare in Georgia is provided by a universal health care system under which the state funds medical treatment in a mainly privatized system of medical facilities. In 2013, the enactment of a universal health care program triggered universal coverage of government-sponsored medical care of the population and improving access to health care services. Responsibility for purchasing publicly financed health services lies with the Social Service Agency (SSA).
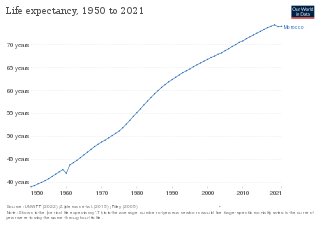
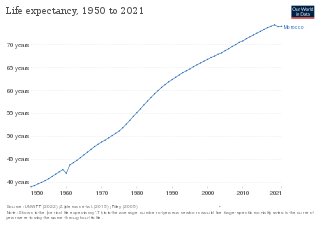
Botswana's healthcare system has been steadily improving and expanding its infrastructure to become more accessible. The country's position as an upper middle-income country has allowed them to make strides in universal healthcare access for much of Botswana's population. The majority of the Botswana's 2.3 million inhabitants now live within five kilometres of a healthcare facility. As a result, the infant mortality and maternal mortality rates have been on a steady decline. The country's improving healthcare infrastructure has also been reflected in an increase of the average life expectancy from birth, with nearly all births occurring in healthcare facilities.
The Republic of Moldova has a universal health care system.

Examples of health care systems of the world, sorted by continent, are as follows.
The WHO's estimate of life expectancy for a female child born in Guinea-Bissau in 2008 was 49 years, and 47 years for a boy. in 2016 life expectancy had improved to 58 for men and 61 for women.
The fertility rate was approximately 3.7 per woman in Honduras in 2009. The under-five mortality rate is at 40 per 1,000 live births. The health expenditure was US$197 per person in 2004. There are about 57 physicians per 100,000 people.

As of 2019 Lithuanian life expectancy at birth was 76.0 and the infant mortality rate was 2.99 per 1,000 births. This is below the EU and OECD average.
Jamaica’s health care has had a weak history, however has been improving and continuing to improve. Part of this is from the fact that close to half of the healthcare workers from the area are leaving for the better opportunities that are offered elsewhere. The other cause comes from Jamaica’s history. Jamaica’s weak healthcare started back when Jamaica was still a colony that depended on slaves, and has been slowly improving ever since. Covid-19 and sickle cell have impacted Jamaica heavily, but their statistics continue to improve. Jamaica has gotten help from various countries and corporations to improve their healthcare system.