Enteritis is inflammation of the small intestine. It is most commonly caused by food or drink contaminated with pathogenic microbes, such as Serratia, but may have other causes such as NSAIDs, radiation therapy as well as autoimmune conditions like coeliac disease. Symptoms may include abdominal pain, cramping, diarrhoea, dehydration, and fever. Related diseases of the gastrointestinal (GI) system may involve inflammation of the stomach and large intestine.
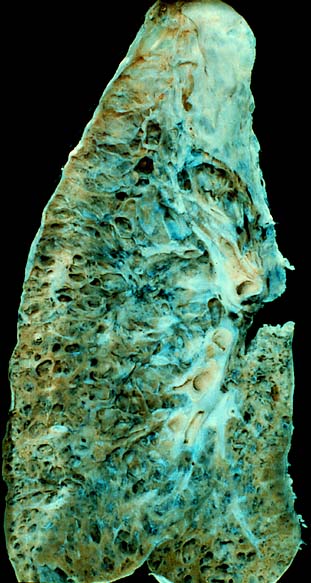
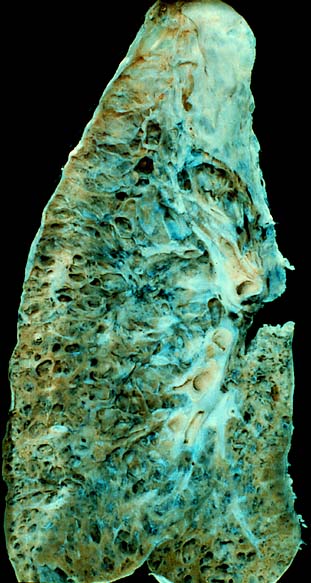
Interstitial lung disease (ILD), or diffuse parenchymal lung disease (DPLD), is a group of respiratory diseases affecting the interstitium and space around the alveoli of the lungs. It concerns alveolar epithelium, pulmonary capillary endothelium, basement membrane, and perivascular and perilymphatic tissues. It may occur when an injury to the lungs triggers an abnormal healing response. Ordinarily, the body generates just the right amount of tissue to repair damage, but in interstitial lung disease, the repair process is disrupted, and the tissue around the air sacs (alveoli) becomes scarred and thickened. This makes it more difficult for oxygen to pass into the bloodstream. The disease presents itself with the following symptoms: shortness of breath, nonproductive coughing, fatigue, and weight loss, which tend to develop slowly, over several months. The average rate of survival for someone with this disease is between three and five years. The term ILD is used to distinguish these diseases from obstructive airways diseases.
Intestinal malrotation is a congenital anomaly of rotation of the midgut. It occurs during the first trimester as the fetal gut undergoes a complex series of growth and development. Malrotation can lead to a dangerous complication called volvulus, in which cases emergency surgery is indicated. Malrotation can refer to a spectrum of abnormal intestinal positioning, often including:

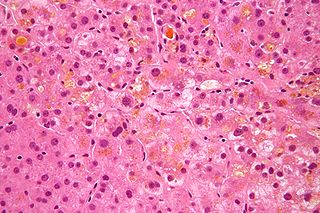
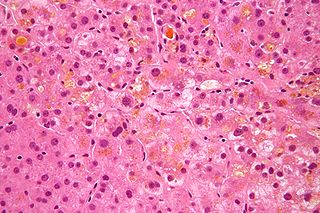
Liver biopsy is the biopsy from the liver. It is a medical test that is done to aid diagnosis of liver disease, to assess the severity of known liver disease, and to monitor the progress of treatment.
Cholestasis is a condition where the flow of bile from the liver to the duodenum is impaired. The two basic distinctions are:

Mediastinitis is inflammation of the tissues in the mid-chest, or mediastinum. It can be either acute or chronic. It is thought to be due to four different etiologies:
Retroperitoneal fibrosis or Ormond's disease is a disease featuring the proliferation of fibrous tissue (fibrosis) in the retroperitoneum, the compartment of the body containing the kidneys, aorta, renal tract, and various other structures. It may present with lower back pain, kidney failure, hypertension, deep vein thrombosis, and other obstructive symptoms. It is named after John Kelso Ormond, who rediscovered the condition in 1948.

Lymphangiectasia, also known as "lymphangiectasis", is a pathologic dilation of lymph vessels. When it occurs in the intestines it is known as intestinal lymphangiectasia, colloquially recognized as Waldmann's disease in cases where there is no secondary cause. The primary defect lies in the inability of the lymphatic system to adequately drain lymph, resulting in its subsequent accumulation and leakage into the intestinal lumen. This condition, first described by Waldmann in 1961, is typically diagnosed in infancy or early childhood. However, it can also manifest in adults, exhibiting a broad spectrum of clinical symptoms.

Intestinal pseudo-obstruction (IPO) is a clinical syndrome caused by severe impairment in the ability of the intestines to push food through. It is characterized by the signs and symptoms of intestinal obstruction without any lesion in the intestinal lumen. Clinical features mimic those seen with mechanical intestinal obstructions and can include abdominal pain, nausea, abdominal distension, vomiting, dysphagia and constipation depending upon the part of the gastrointestinal tract involved.

Autoimmune Pancreatitis (AIP) is an increasingly recognized type of chronic pancreatitis that can be difficult to distinguish from pancreatic carcinoma but which responds to treatment with corticosteroids, particularly prednisone. Although autoimmune pancreatitis is quite rare, it constitutes an important clinical problem for both patients and their clinicians: the disease commonly presents itself as a tumorous mass which is diagnostically indistinguishable from pancreatic cancer, a disease that is much more common in addition to being very dangerous. Hence, some patients undergo pancreatic surgery, which is associated to substantial mortality and morbidity, out of the fear by patients and clinicians to undertreat a malignancy. However, surgery is not a good treatment for this condition as AIP responds well to immunosuppressive treatment. There are two categories of AIP: Type 1 and Type 2, each with distinct clinical profiles.

Bowel infarction or gangrenous bowel represents an irreversible injury to the intestine resulting from insufficient blood flow. It is considered a medical emergency because it can quickly result in life-threatening infection and death. Any cause of bowel ischemia, the earlier reversible form of injury, may ultimately lead to infarction if uncorrected. The causes of bowel ischemia or infarction include primary vascular causes and other causes of bowel obstruction.
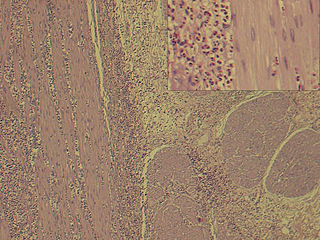
Eosinophilic gastroenteritis, also known as eosinophilic enteritis, is a rare and heterogeneous condition characterized by patchy or diffuse eosinophilic infiltration of gastrointestinal (GI) tissue, first described by Kaijser in 1937. Presentation may vary depending on location as well as depth and extent of bowel wall involvement and usually runs a chronic relapsing course. It can be classified into mucosal, muscular and serosal types based on the depth of involvement. Any part of the GI tract can be affected, and isolated biliary tract involvement has also been reported. The stomach is the organ most commonly affected, followed by the small intestine and the colon.

Intestinal ischemia is a medical condition in which injury to the large or small intestine occurs due to not enough blood supply. It can come on suddenly, known as acute intestinal ischemia, or gradually, known as chronic intestinal ischemia. The acute form of the disease often presents with sudden severe abdominal pain and is associated with a high risk of death. The chronic form typically presents more gradually with abdominal pain after eating, unintentional weight loss, vomiting, and fear of eating.

SeHCAT is a drug used in a clinical test to diagnose bile acid malabsorption.
Secondary sclerosing cholangitis (SSC) is a chronic cholestatic liver disease. SSC is a sclerosing cholangitis with a known cause. Alternatively, if no cause can be identified, then primary sclerosing cholangitis is diagnosed. SSC is an aggressive and rare disease with complex and multiple causes. It is characterized by inflammation, fibrosis, destruction of the biliary tree and biliary cirrhosis. It can be treated with minor interventions such as continued antibiotic use and monitoring, or in more serious cases, laparoscopic surgery intervention, and possibly a liver transplant.
Acquired generalized lipodystrophy (AGL), also known as Lawrence syndrome and Lawrence–Seip syndrome, is a rare skin condition that appears during childhood or adolescence, characterized by fat loss affecting large areas of the body, particularly the face, arms, and legs. There are four types of lipodystrophy based on its onset and areas affected: acquired or inherited, and generalized or partial. Both acquired or inherited lipodystrophy present as loss of adipose tissues, in the absence of nutritional deprivation. The near-total loss of subcutaneous adipose tissue is termed generalized lipodystrophy while the selective loss of adipose tissues is denoted as partial lipodystrophy. Thus, as the name suggests, AGL is a near-total deficiency of adipose tissues in the body that is developed later in life. It is an extremely rare disease with only about 100 cases reported worldwide. There are three main etiologies of AGL suspected: autoimmune, panniculitis-associated, or idiopathic. After its onset, the disease progresses over a few days, weeks, months, or even in years. Clinical presentations of AGL are similar to other lipodystrophies, including metabolic complications and hypoleptinemia. Treatments are also similar and mainly supportive for symptomatic alleviation. Although HIV- or drug-induced lipodystrophy are types of acquired lipodystrophy, their origins are very specific and distinct and hence are usually not discussed with AGL.
Waldmann disease, also known as Primary Intestinal Lymphangiectasia (PIL), is a rare disease characterized by enlargement of the lymph vessels supplying the lamina propria of the small intestine. Although its prevalence is unknown, it being classified as a "rare disease" means that less than 200,000 of the population of the United States are affected by this condition and its subtypes and there have been approximately 50 reported cases of adult-onset PIL since 1961.
Bile acid malabsorption (BAM), known also as bile acid diarrhea, is a cause of several gut-related problems, the main one being chronic diarrhea. It has also been called bile acid-induced diarrhea, cholerheic or choleretic enteropathy, bile salt diarrhea or bile salt malabsorption. It can result from malabsorption secondary to gastrointestinal disease, or be a primary disorder, associated with excessive bile acid production. Treatment with bile acid sequestrants is often effective. Depending on the severity of symptoms, it may be recognised as a disability in the United Kingdom under the Equality Act 2010.

IgG4-related disease (IgG4-RD), formerly known as IgG4-related systemic disease, is a chronic inflammatory condition characterized by tissue infiltration with lymphocytes and IgG4-secreting plasma cells, various degrees of fibrosis (scarring) and a usually prompt response to oral steroids. In approximately 51–70% of people with this disease, serum IgG4 concentrations are elevated during an acute phase.
The comb sign is a radiological sign seen on computed tomography or magnetic resonance imaging scans, primarily used to identify inflammation in the mesentery. It refers to the appearance of engorged mesenteric vessels resembling the teeth of a comb, which is a key feature seen in several abdominal conditions, particularly those associated with inflammatory bowel diseases, such as Crohn's disease. This sign was first described by Dr. Morton Mayers.