Related Research Articles

A local anesthetic (LA) is a medication that causes absence of all sensation in a specific body part without loss of consciousness, as opposed to a general anesthetic, which eliminates all sensation in the entire body and causes unconsciousness. Local anesthetics are most commonly used to eliminate pain during or after surgery. When it is used on specific nerve pathways, paralysis also can be induced.

Spinal anaesthesia, also called spinal block, subarachnoid block, intradural block and intrathecal block, is a form of neuraxial regional anaesthesia involving the injection of a local anaesthetic or opioid into the subarachnoid space, generally through a fine needle, usually 9 cm (3.5 in) long. It is a safe and effective form of anesthesia usually performed by anesthesiologists that can be used as an alternative to general anesthesia commonly in surgeries involving the lower extremities and surgeries below the umbilicus. The local anesthetic with or without an opioid injected into the cerebrospinal fluid provides locoregional anaesthesia: true analgesia, motor, sensory and autonomic (sympathetic) blockade. Administering analgesics in the cerebrospinal fluid without a local anaesthetic produces locoregional analgesia: markedly reduced pain sensation, some autonomic blockade, but no sensory or motor block. Locoregional analgesia, due to mainly the absence of motor and sympathetic block may be preferred over locoregional anaesthesia in some postoperative care settings. The tip of the spinal needle has a point or small bevel. Recently, pencil point needles have been made available.

Alveolar osteitis, also known as dry socket, is inflammation of the alveolar bone. Classically, this occurs as a postoperative complication of tooth extraction.

The inferior alveolar nerve (IAN) (also the inferior dental nerve) is a sensory branch of the mandibular nerve (CN V3) (which is itself the third branch of the trigeminal nerve (CN V)). The nerve provides sensory innervation to the lower/mandibular teeth and their corresponding gingiva as well as a small area of the face (via its mental nerve).

A dental extraction is the removal of teeth from the dental alveolus (socket) in the alveolar bone. Extractions are performed for a wide variety of reasons, but most commonly to remove teeth which have become unrestorable through tooth decay, periodontal disease, or dental trauma, especially when they are associated with toothache. Sometimes impacted wisdom teeth cause recurrent infections of the gum (pericoronitis), and may be removed when other conservative treatments have failed. In orthodontics, if the teeth are crowded, healthy teeth may be extracted to create space so the rest of the teeth can be straightened.

The alveolar process or alveolar bone is the thickened ridge of bone that contains the tooth sockets on the jaw bones. The structures are covered by gums as part of the oral cavity.
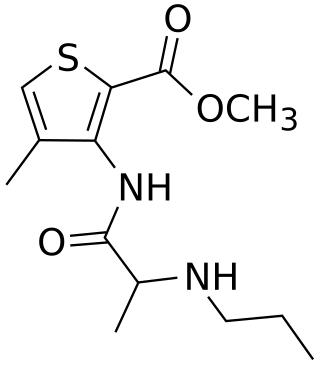
Articaine is a dental amide-type local anesthetic. It is the most widely used local anesthetic in a number of European countries and is available in many countries. It is the only local anaesthetic to contain a thiophene ring, meaning it can be described as 'thiophenic'; this conveys lipid solubility.

The lingual nerve carries sensory innervation from the anterior two-thirds of the tongue. It contains fibres from both the mandibular division of the trigeminal nerve (CN V3) and from the facial nerve (CN VII). The fibres from the trigeminal nerve are for touch, pain and temperature (general sensation), and the ones from the facial nerve are for taste (special sensation).

The mental nerve is a sensory nerve of the face. It is a branch of the posterior trunk of the inferior alveolar nerve, itself a branch of the mandibular nerve (CN V3), itself a branch of the trigeminal nerve (CN V). It provides sensation to the front of the chin and the lower lip, as well as the gums of the anterior mandibular (lower) teeth. It can be blocked with local anaesthesia for procedures on the chin, lower lip, and mucous membrane of the inner cheek. Problems with the nerve cause chin numbness.

Dental instruments are tools that dental professionals use to provide dental treatment. They include tools to examine, manipulate, treat, restore, and remove teeth and surrounding oral structures.
Dental anesthesia is the application of anesthesia to dentistry. It includes local anesthetics, sedation, and general anesthesia.
Dental pertains to the teeth, including dentistry. Topics related to the dentistry, the human mouth and teeth include:

When extracting lower wisdom teeth, coronectomy is a treatment option involving removing the crown of the lower wisdom tooth, whilst keeping the roots in place in healthy patients. This option is given to patients as an alternative to extraction when the wisdom teeth are in close association with the inferior alveolar nerve, and so used to prevent damage to the nerve which may occur during extraction.
Inferior alveolar nerve block is a nerve block technique which induces anesthesia (numbness) in the areas of the mouth and face innervated by one of the inferior alveolar nerves which are paired on the left and right side. These areas are the skin and mucous membranes of the lower lip, the skin of the chin, the lower teeth and the labial gingiva of the anterior teeth, all unilaterally to the midline of the side on which the block is administered. However, depending on technique, the long buccal nerve may not be anesthetized by an IANB and therefore an area of buccal gingiva adjacent to the lower posterior teeth will retain normal sensation unless that nerve is anesthetized separately, via a (long) buccal nerve block. The inferior alveolar nerve is a branch of the mandibular nerve, the third division of the trigeminal nerve. This procedure attempts to anaesthetise the inferior alveolar nerve prior to it entering the mandibular foramen on the medial surface of the mandibular ramus.

In dentistry, a furcation defect is bone loss, usually a result of periodontal disease, affecting the base of the root trunk of a tooth where two or more roots meet. The extent and configuration of the defect are factors in both diagnosis and treatment planning.
The following outline is provided as an overview of and topical guide to anesthesia:

In human anatomy, the mouth is the first portion of the alimentary canal that receives food and produces saliva. The oral mucosa is the mucous membrane epithelium lining the inside of the mouth.
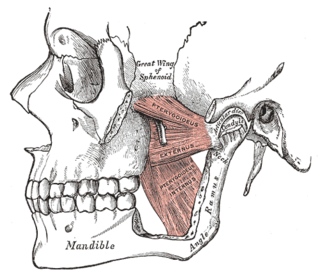
The pterygomandibular space is a fascial space of the head and neck. It is a potential space in the head and is paired on each side. It is located between the lateral pterygoid muscle and the medial surface of the ramus of the mandible. The pterygomandibular space is one of the four compartments of the masticator space.
Alveoloplasty is a surgical pre-prosthetic procedure performed to facilitate removal of teeth, and smoothen or reshape the jawbone for prosthetic and cosmetic purposes. In this procedure, the bony edges of the alveolar ridge and its surrounding structures is made smooth, redesigned or recontoured so that a well-fitting, comfortable, and esthetic prosthesis may be fabricated or implants may be surgically inserted. This pre-prosthetic surgery which may include bone grafting prepares the mouth to receive a prosthesis or implants by improving the condition and quality of the supporting structures so they can provide support, better retention and stability to the prosthesis.

Caudal anaesthesia is a form of neuraxial regional anaesthesia conducted by accessing the epidural space via the sacral hiatus. It is typically used in paediatrics to provide peri- and post-operative analgesia for surgeries below the umbilicus. In adults it is used for chronic low back pain management.
References
- ↑ Campoy, Luis; Read, Matt (2012). Small Animal Regional Anesthesia and Analgesia. John Wiley & Sons. ISBN 9781118507902 . Retrieved 5 December 2017.
- ↑ Duggal, M. S.; Curzon, M. E. J.; Fayle, S. A.; Toynba, K. J.; Robertson, A. J. (2002). Restorative Techniques in Paediatric Dentistry: An Illustrated Guide to the Restoration of Extensive Carious Primary Teeth. CRC Press. p. 23. ISBN 9781853175923 . Retrieved 5 December 2017.
- ↑ PhillipsWH. Anatomic considerations in local anesthesia. J Oral Surg.1943;1:112^121.
- ↑ Reed, Kenneth L.; Malamed, Stanley F.; Fonner, Andrea M. (2012). "Local Anesthesia Part 2: Technical Considerations". Anesthesia Progress. 59 (3): 127–137. doi:10.2344/0003-3006-59.3.127. PMC 3468291 . PMID 23050753.
- 1 2 3 Local anesthesia in dentistry. Baart, Jacques A.,, Brand, Henk S. (Second ed.). Cham. 26 June 2017. ISBN 9783319437040. OCLC 989726183.
{{cite book}}: CS1 maint: location missing publisher (link) CS1 maint: others (link) - 1 2 3 4 5 Anesthesia complications in the dental office. Bosack, Robert C.,, Lieblich, Stuart E. Ames, Iowa. 15 June 2015. ISBN 9780470960295. OCLC 900159251.
{{cite book}}: CS1 maint: location missing publisher (link) CS1 maint: others (link) - 1 2 3 4 5 A., Baart, J. (2009). Local Anaesthesia in Dentistry. Brand, H. S. Chichester: John Wiley & Sons. ISBN 9781444309577. OCLC 437112327.
{{cite book}}: CS1 maint: multiple names: authors list (link) - ↑ Lee, Jiseon; Lee, Ju-Young; Kim, Hyun Jeong; Seo, Kwang-Suk (September 2016). "Dental anesthesia for patients with allergic reactions to lidocaine: two case reports". Journal of Dental Anesthesia and Pain Medicine. 16 (3): 209–212. doi:10.17245/jdapm.2016.16.3.209. PMC 5586559 . PMID 28884155.