
A goitre, or goiter, is a swelling in the neck resulting from an enlarged thyroid gland. A goitre can be associated with a thyroid that is not functioning properly.

Hyperthyroidism is the condition that occurs due to excessive production of thyroid hormones by the thyroid gland. Thyrotoxicosis is the condition that occurs due to excessive thyroid hormone of any cause and therefore includes hyperthyroidism. Some, however, use the terms interchangeably. Signs and symptoms vary between people and may include irritability, muscle weakness, sleeping problems, a fast heartbeat, heat intolerance, diarrhea, enlargement of the thyroid, hand tremor, and weight loss. Symptoms are typically less severe in the elderly and during pregnancy. An uncommon complication is thyroid storm in which an event such as an infection results in worsening symptoms such as confusion and a high temperature and often results in death. The opposite is hypothyroidism, when the thyroid gland does not make enough thyroid hormone.

The thyroid, or thyroid gland, is an endocrine gland in the neck consisting of two connected lobes. The lower two thirds of the lobes are connected by a thin band of tissue called the thyroid isthmus. The thyroid is located at the front of the neck, below the Adam's apple. Microscopically, the functional unit of the thyroid gland is the spherical thyroid follicle, lined with follicular cells (thyrocytes), and occasional parafollicular cells that surround a lumen containing colloid. The thyroid gland secretes three hormones: the two thyroid hormones – triiodothyronine (T3) and thyroxine (T4) – and a peptide hormone, calcitonin. The thyroid hormones influence the metabolic rate and protein synthesis, and in children, growth and development. Calcitonin plays a role in calcium homeostasis. Secretion of the two thyroid hormones is regulated by thyroid-stimulating hormone (TSH), which is secreted from the anterior pituitary gland. TSH is regulated by thyrotropin-releasing hormone (TRH), which is produced by the hypothalamus.
Hypothyroidism, also called underactive thyroid or low thyroid, is a disorder of the endocrine system in which the thyroid gland does not produce enough thyroid hormone. It can cause a number of symptoms, such as poor ability to tolerate cold, a feeling of tiredness, constipation, slow heart rate, depression, and weight gain. Occasionally there may be swelling of the front part of the neck due to goiter. Untreated cases of hypothyroidism during pregnancy can lead to delays in growth and intellectual development in the baby or congenital iodine deficiency syndrome.

Adrenal insufficiency is a condition in which the adrenal glands do not produce adequate amounts of steroid hormones, primarily cortisol; but may also include impaired production of aldosterone, which regulates sodium conservation, potassium secretion, and water retention. Craving for salt or salty foods due to the urinary losses of sodium is common.

Achlorhydria, also known as hypochlorhydria, refers to states where the production of hydrochloric acid in gastric secretions of the stomach and other digestive organs is absent or low, respectively. It is associated with various other medical problems.
Inborn errors of metabolism form a large class of genetic diseases involving congenital disorders of metabolism. The majority are due to defects of single genes that code for enzymes that facilitate conversion of various substances (substrates) into others (products). In most of the disorders, problems arise due to accumulation of substances which are toxic or interfere with normal function, or to the effects of reduced ability to synthesize essential compounds. Inborn errors of metabolism are now often referred to as congenital metabolic diseases or inherited metabolic disorders. The term inborn errors of metabolism was coined by a British physician, Archibald Garrod (1857–1936), in 1908. He is known for work that prefigured the "one gene-one enzyme" hypothesis, based on his studies on the nature and inheritance of alkaptonuria. His seminal text, Inborn Errors of Metabolism was published in 1923.
The Jod-Basedow effect is hyperthyroidism following administration of iodine or iodide, either as a dietary supplement or as iodinated contrast for medical imaging.
This is a shortened version of the third chapter of the ICD-10: Diseases of the blood and blood-forming organs, and certain disorders involving the immune mechanism. It covers ICD codes D50.0 to D89.9. All versions of the ICD-10, including the most recent one (2019), can be browsed freely on the website of the World Health Organisation (WHO). The ICD-10 can also be downloaded in PDF-form.

Endocrine diseases are disorders of the endocrine system. The branch of medicine associated with endocrine disorders is known as endocrinology.

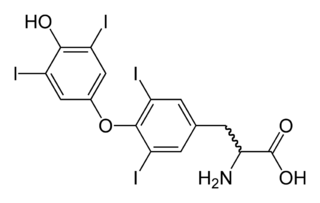
Thyroid hormones are two hormones produced and released by the thyroid gland, namely triiodothyronine (T3) and thyroxine (T4). They are tyrosine-based hormones that are primarily responsible for regulation of metabolism. T3 and T4 are partially composed of iodine. A deficiency of iodine leads to decreased production of T3 and T4, enlarges the thyroid tissue and will cause the disease known as simple goitre. The major form of thyroid hormone in the blood is thyroxine (T4), which has a longer half-life than T3. In humans, the ratio of T4 to T3 released into the blood is approximately 14:1. T4 is converted to the active T3 (three to four times more potent than T4) within cells by deiodinases (5′-iodinase). These are further processed by decarboxylation and deiodination to produce iodothyronamine (T1a) and thyronamine (T0a). All three isoforms of the deiodinases are selenium-containing enzymes, thus dietary selenium is essential for T3 production.

The kynurenine pathway is a metabolic pathway leading to the production of nicotinamide adenine dinucleotide (NAD+), as well as other active metabolites, from the degradation of tryptophan, an essential amino acid. Disruption in the pathway is associated with certain genetic disorders.
Complications of diabetes mellitus include problems that develop rapidly (acute) or over time (chronic) and may affect many organ systems. The complications of diabetes can dramatically impair quality of life and cause long-lasting disability. Overall, complications are far less common and less severe in people with well-controlled blood sugar levels. Some non-modifiable risk factors such as age at diabetes onset, type of diabetes, gender and genetics may influence risk. Other health problems compound the chronic complications of diabetes such as smoking, obesity, high blood pressure, elevated cholesterol levels, and lack of regular exercise.
Thyroid disease in pregnancy can affect the health of the mother as well as the child before and after delivery. Thyroid disorders are prevalent in women of child-bearing age and for this reason commonly present as a pre-existing disease in pregnancy, or after childbirth. Uncorrected thyroid dysfunction in pregnancy has adverse effects on fetal and maternal well-being. The deleterious effects of thyroid dysfunction can also extend beyond pregnancy and delivery to affect neurointellectual development in the early life of the child. Due to an increase in thyroxine binding globulin, an increase in placental type 3 deioidinase and the placental transfer of maternal thyroxine to the fetus, the demand for thyroid hormones is increased during pregnancy. The necessary increase in thyroid hormone production is facilitated by high human chorionic gonadotropin (hCG) concentrations, which bind the TSH receptor and stimulate the maternal thyroid to increase maternal thyroid hormone concentrations by roughly 50%. If the necessary increase in thyroid function cannot be met, this may cause a previously unnoticed (mild) thyroid disorder to worsen and become evident as gestational thyroid disease. Currently, there is not enough evidence to suggest that screening for thyroid dysfunction is beneficial, especially since treatment thyroid hormone supplementation may come with a risk of overtreatment. After women give birth, about 5% develop postpartum thyroiditis which can occur up to nine months afterwards.This is characterized by a short period of hyperthyroidism followed by a period of hypothyroidism; 20–40% remain permanently hypothyroid.
Thyroid's secretory capacity is the maximum stimulated amount of thyroxine that the thyroid can produce in a given time-unit.
The sum activity of peripheral deiodinases is the maximum amount of triiodothyronine produced per time-unit under conditions of substrate saturation. It is assumed to reflect the activity of deiodinases outside the central nervous system and other isolated compartments. GD is therefore expected to reflect predominantly the activity of type I deiodinase.