| Aqueous humour | |
|---|---|
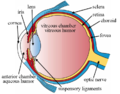
 Schematic diagram of the human eye. | |
| Details | |
| Identifiers | |
| Latin | humor aquosus |
| MeSH | D001082 |
| TA98 | A15.2.06.002 |
| TA2 | 6791 |
| FMA | 58819 |
| Anatomical terminology | |
The aqueous humour is a transparent water-like fluid similar to blood plasma, but containing low protein concentrations. It is secreted from the ciliary body, a structure supporting the lens of the eyeball. [1] It fills both the anterior and the posterior chambers of the eye, and is not to be confused with the vitreous humour, which is located in the space between the lens and the retina, also known as the posterior cavity or vitreous chamber. [2] Blood cannot normally enter the eyeball. [3]
Contents
- Structure
- Composition
- Function
- Production
- Drainage
- Clinical significance
- Additional images
- See also
- References
- External links
#We find the structure called iris behind the cornea.Iris is a dark muscular diaphragm that controls the size of the pupil .
@The pupil regulates and controls the amount of light entering the eye .
&The eye lens forms an inverted real image of the object on the retina.
/The retina is a delicate membrane having enormous no.of light sensitive cells .
(The light-sensitive cells get activated upon illumination and generate electrical system of Eye signals.)