Glaucoma is a group of eye diseases that can lead to damage of the optic nerve. The optic nerve transmits visual information from the eye to the brain. Glaucoma may cause vision loss if left untreated. It has been called the "silent thief of sight" because the loss of vision usually occurs slowly over a long period of time. A major risk factor for glaucoma is increased pressure within the eye, known as intraocular pressure (IOP). It is associated with old age, a family history of glaucoma, and certain medical conditions or the use of some medications. The word glaucoma comes from the Ancient Greek word γλαυκός, meaning 'gleaming, blue-green, gray'.

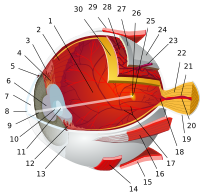
In neuroanatomy, the optic nerve, also known as the second cranial nerve, cranial nerve II, or simply CN II, is a paired cranial nerve that transmits visual information from the retina to the brain. In humans, the optic nerve is derived from optic stalks during the seventh week of development and is composed of retinal ganglion cell axons and glial cells; it extends from the optic disc to the optic chiasma and continues as the optic tract to the lateral geniculate nucleus, pretectal nuclei, and superior colliculus.

Papilledema or papilloedema is optic disc swelling that is caused by increased intracranial pressure due to any cause. The swelling is usually bilateral and can occur over a period of hours to weeks. Unilateral presentation is extremely rare.
The visual field is "that portion of space in which objects are visible at the same moment during steady fixation of the gaze in one direction"; in ophthalmology and neurology the emphasis is mostly on the structure inside the visual field and it is then considered “the field of functional capacity obtained and recorded by means of perimetry”.

The optic disc or optic nerve head is the point of exit for ganglion cell axons leaving the eye. Because there are no rods or cones overlying the optic disc, it corresponds to a small blind spot in each eye.

A coloboma is a hole in one of the structures of the eye, such as the iris, retina, choroid, or optic disc. The hole is present from birth and can be caused when a gap called the choroid fissure, which is present during early stages of prenatal development, fails to close up completely before a child is born. Ocular coloboma is relatively uncommon, affecting less than one in every 10,000 births.
Dominant optic atrophy (DOA), or autosomal dominant optic atrophy (ADOA), (Kjer's type) is an autosomally inherited disease that affects the optic nerves, causing reduced visual acuity and blindness beginning in childhood. However, the disease can seem to re-present a second time with further vision loss due to the early onset of presbyopia symptoms (i.e., difficulty in viewing objects up close). DOA is characterized as affecting neurons called retinal ganglion cells (RGCs). This condition is due to mitochondrial dysfunction mediating the death of optic nerve fibers. The RGCs axons form the optic nerve. Therefore, the disease can be considered of the central nervous system. Dominant optic atrophy was first described clinically by Batten in 1896 and named Kjer’s optic neuropathy in 1959 after Danish ophthalmologist Poul Kjer, who studied 19 families with the disease. Although dominant optic atrophy is the most common autosomally inherited optic neuropathy (i.e., disease of the optic nerves), it is often misdiagnosed.

Pigment dispersion syndrome (PDS) is an eye disorder that can lead to a form of glaucoma known as pigmentary glaucoma. It takes place when pigment cells slough off from the back of the iris and float around in the aqueous humor. Over time, these pigment cells can accumulate in the anterior chamber in such a way that they begin to clog the trabecular meshwork, which can in turn prevent the aqueous humour from draining and therefore increases the pressure inside the eye. A common finding in PDS are central, vertical corneal endothelial pigment deposits, known as Krukenberg spindle. With PDS, the intraocular pressure tends to spike at times and then can return to normal. Exercise has been shown to contribute to spikes in pressure as well. When the pressure is great enough to cause damage to the optic nerve, this is called pigmentary glaucoma. As with all types of glaucoma, when damage happens to the optic nerve fibers, the vision loss that occurs is irreversible and painless.

The retinal nerve fiber layer (RNFL) or nerve fiber layer, stratum opticum, is part of the anatomy of the eye.

Dilated fundus examination (DFE) is a diagnostic procedure that uses mydriatic eye drops to dilate or enlarge the pupil in order to obtain a better view of the fundus of the eye. Once the pupil is dilated, examiners use ophthalmoscopy to view the eye's interior, which makes it easier to assess the retina, optic nerve head, blood vessels, and other important features. DFE has been found to be a more effective method for evaluating eye health when compared to non-dilated examination, and is the best method of evaluating structures behind the iris. It is frequently performed by ophthalmologists and optometrists as part of an eye examination.
Optic neuropathy is damage to the optic nerve from any cause. The optic nerve is a bundle of millions of fibers in the retina that sends visual signals to the brain.

Papillorenal syndrome is an autosomal dominant genetic disorder marked by underdevelopment (hypoplasia) of the kidney and colobomas of the optic nerve.

Optic disc drusen (ODD) are globules of mucoproteins and mucopolysaccharides that progressively calcify in the optic disc. They are thought to be the remnants of the axonal transport system of degenerated retinal ganglion cells. ODD have also been referred to as congenitally elevated or anomalous discs, pseudopapilledema, pseudoneuritis, buried disc drusen, and disc hyaline bodies.

Optic pit, optic nerve pit, or optic disc pit (ODP) is rare a congenital excavation (or regional depression) of the optic disc (also optic nerve head), resulting from a malformation during development of the eye. The incidence of ODP is 1 in 10,000 people with no predilection for either gender. There is currently no known risk factors for their development. Optic pits are important because they are associated with posterior vitreous detachments (PVD) and even serous retinal detachments.
Sohan Singh Hayreh was an ophthalmologist, clinical scientist, and professor emeritus of ophthalmology at the University of Iowa. As one of the pioneers in the field of fluorescein angiography, he was generally acknowledged to be a leading authority in vascular diseases of the eye and the optic nerve. For over 60 years, Hayreh was actively involved in basic, experimental, and clinical research in ophthalmology, publishing over 400 original peer-reviewed articles in various international ophthalmic journals, six classical monographs and books in his field of research, and more than 50 chapters in ophthalmic books. He made many seminal observations dealing with the ocular circulation in health and disease, the optic disc and the optic nerve, retinal and choroidal vascular disorders, glaucomatous optic neuropathy, fundus changes in malignant arterial hypertension, ocular neovascularization, rheumatologic disorders of the eye, and nocturnal arterial hypotension. He was an elected fellow of the National Academy of Medical Sciences.
Normal tension glaucoma (NTG) is an eye disease, a neuropathy of the optic nerve, that shows all the characteristics of primary open angle glaucoma except one: the elevated intraocular pressure (IOP) - the classic hallmark of glaucoma - is missing. Normal tension glaucoma is in many cases closely associated with general issues of blood circulation and of organ perfusion like arterial hypotension, metabolic syndrome, and Flammer syndrome.

James C. Tsai is a physician and scientist who serves as president of the New York Eye and Ear Infirmary of Mount Sinai. He also serves as the Delafield-Rodgers Professor of Ophthalmology at the Icahn School of Medicine at Mount Sinai and chair of the department of ophthalmology at the Mount Sinai Health System.

Helen Victoria Danesh-Meyer is a New Zealand ophthalmology academic, and as of 2008 is a full professor at the University of Auckland.
Megalopapilla is a non-progressive human eye condition in which the optic nerve head has an enlarged diameter, exceeding 2.1 mm with no other morphological abnormalities.

The Heidelberg Retinal Tomography is a diagnostic procedure used in ophthalmology. The Heidelberg Retina Tomograph (HRT) is an ophthalmological confocal point scanning laser ophthalmoscope for examining the cornea and certain areas of the retina using different diagnostic modules. However, the most widely used area of application for HRT is the inspection of the optic nerve head (papilla) for early detection and follow-up of glaucoma. The procedure has established itself as an integral part of routine glaucoma diagnostics alongside the visual field examination (perimetry), the chamber angle examination (gonioscopy) and the measurement of intraocular pressure (tonometry). The HRT is the most widely used application of confocal scanning laser ophthalmoscopy.