Edema, also spelled oedema, and also known as fluid retention, dropsy and hydropsy, is the build-up of fluid in the body's tissue, a type of swelling. Most commonly, the legs or arms are affected. Symptoms may include skin that feels tight, the area feeling heavy, and joint stiffness. Other symptoms depend on the underlying cause.
Hyponatremia or hyponatraemia is a low concentration of sodium in the blood. It is generally defined as a sodium concentration of less than 135 mmol/L (135 mEq/L), with severe hyponatremia being below 120 mEq/L. Symptoms can be absent, mild or severe. Mild symptoms include a decreased ability to think, headaches, nausea, and poor balance. Severe symptoms include confusion, seizures, and coma; death can ensue.

Heart failure (HF), also known as congestive heart failure (CHF), is a syndrome caused by an impairment in the heart's ability to fill with and pump blood.

Nephrotic syndrome is a collection of symptoms due to kidney damage. This includes protein in the urine, low blood albumin levels, high blood lipids, and significant swelling. Other symptoms may include weight gain, feeling tired, and foamy urine. Complications may include blood clots, infections, and high blood pressure.

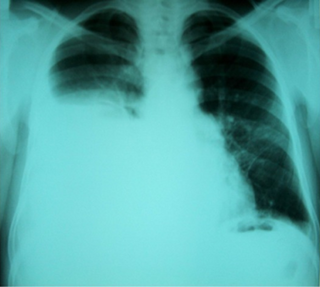
Pulmonary edema, also known as pulmonary congestion, is excessive fluid accumulation in the tissue or air spaces of the lungs. This leads to impaired gas exchange, most often leading to shortness of breath (dyspnea) which can progress to hypoxemia and respiratory failure. Pulmonary edema has multiple causes and is traditionally classified as cardiogenic or noncardiogenic.

Electrolyte imbalance, or water-electrolyte imbalance, is an abnormality in the concentration of electrolytes in the body. Electrolytes play a vital role in maintaining homeostasis in the body. They help to regulate heart and neurological function, fluid balance, oxygen delivery, acid–base balance and much more. Electrolyte imbalances can develop by consuming too little or too much electrolyte as well as excreting too little or too much electrolyte. Examples of electrolytes include calcium, chloride, magnesium, phosphate, potassium, and sodium.

Loop diuretics are pharmacological agents that primarily inhibit the Na-K-Cl cotransporter located on the luminal membrane of cells along the thick ascending limb of the loop of Henle. They are often used for the treatment of hypertension and edema secondary to congestive heart failure, liver cirrhosis, or chronic kidney disease. While thiazide diuretics are more effective in patients with normal kidney function, loop diuretics are more effective in patients with impaired kidney function.
Hypernatremia, also spelled hypernatraemia, is a high concentration of sodium in the blood. Early symptoms may include a strong feeling of thirst, weakness, nausea, and loss of appetite. Severe symptoms include confusion, muscle twitching, and bleeding in or around the brain. Normal serum sodium levels are 135–145 mmol/L. Hypernatremia is generally defined as a serum sodium level of more than 145 mmol/L. Severe symptoms typically only occur when levels are above 160 mmol/L.
The syndrome of inappropriate antidiuretic hormone secretion (SIADH), also known as the syndrome of inappropriate antidiuresis (SIAD), is characterized by a physiologically inappropriate release of antidiuretic hormone (ADH) either from the posterior pituitary gland, or an abnormal non-pituitary source. Unsuppressed ADH causes a physiologically inappropriate increase in solute-free water being reabsorbed by the tubules of the kidney to the venous circulation leading to hypotonic hyponatremia.

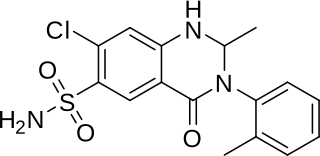
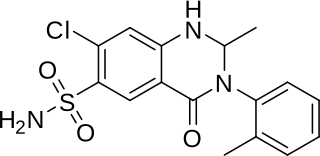
Chlortalidone, also known as chlorthalidone, is a thiazide-like diuretic drug used to treat high blood pressure, swelling, diabetes insipidus, and renal tubular acidosis. Because chlortalidone is effective in most patients with high blood pressure, it is considered a preferred initial treatment. It is also used to prevent calcium-based kidney stones. It is taken by mouth. Effects generally begin within three hours and last for up to three days. Long-term treatment with chlortalidone is more effective than hydrochlorothiazide for prevention of heart attack or stroke.

Conivaptan, sold under the brand name Vaprisol, is a non-peptide inhibitor of the receptor for anti-diuretic hormone, also called vasopressin. It was approved in 2004 for hyponatremia. The compound was discovered by Astellas and marked in 2006. The drug is now marketed by Cumberland Pharmaceuticals, Inc.

Hydrops fetalis or hydrops foetalis is a condition in the fetus characterized by an accumulation of fluid, or edema, in at least two fetal compartments. By comparison, hydrops allantois or hydrops amnion is an accumulation of excessive fluid in the allantoic or amniotic space, respectively.
Metolazone is a thiazide-like diuretic marketed under the brand names Zytanix, Metoz, Zaroxolyn, and Mykrox. It is primarily used to treat congestive heart failure and high blood pressure. Metolazone indirectly decreases the amount of water reabsorbed into the bloodstream by the kidney, so that blood volume decreases and urine volume increases. This lowers blood pressure and prevents excess fluid accumulation in heart failure. Metolazone is sometimes used together with loop diuretics such as furosemide or bumetanide, but these highly effective combinations can lead to dehydration and electrolyte abnormalities.

Osmotherapy is the use of osmotically active substances to reduce the volume of intracranial contents. Osmotherapy serves as the primary medical treatment for cerebral edema. The primary purpose of osmotherapy is to improve elasticity and decrease intracranial volume by removing free water, accumulated as a result of cerebral edema, from brain's extracellular and intracellular space into vascular compartment by creating an osmotic gradient between the blood and brain. Normal serum osmolality ranges from 280 to 290 mOsm/kg and serum osmolality to cause water removal from brain without much side effects ranges from 300 to 320 mOsm/kg. Usually, 90 mL of space is created in the intracranial vault by 1.6% reduction in brain water content. Osmotherapy has cerebral dehydrating effects. The main goal of osmotherapy is to decrease intracranial pressure (ICP) by shifting excess fluid from brain. This is accomplished by intravenous administration of osmotic agents which increase serum osmolality in order to shift excess fluid from intracellular or extracellular space of the brain to intravascular compartment. The resulting brain shrinkage effectively reduces intracranial volume and decreases ICP.
In medicine, intravascular volume status refers to the volume of blood in a patient's circulatory system, and is essentially the blood plasma component of the overall volume status of the body, which otherwise includes both intracellular fluid and extracellular fluid. Still, the intravascular component is usually of primary interest, and volume status is sometimes used synonymously with intravascular volume status.

In transfusion medicine, transfusion-associated circulatory overload is a transfusion reaction resulting in signs or symptoms of excess fluid in the circulatory system (hypervolemia) within 12 hours after transfusion. The symptoms of TACO can include shortness of breath (dyspnea), low blood oxygen levels (hypoxemia), leg swelling, high blood pressure (hypertension), and a high heart rate (tachycardia).
Hypoosmolar hyponatremia is a condition where hyponatremia is associated with a low plasma osmolality. The term "hypotonic hyponatremia" is also sometimes used.
A fluid restriction diet is a diet which limits the amount of daily fluid consumption. Besides beverages, many foods also include fluids which needs to be taken into consideration. A fluid-restrictive diet assists in preventing the build-up of fluids in the body. Reducing fluid intake can alleviate stress on the body and may reduce additional complications. A fluid restriction diet is generally medically advised for patients with "heart problems, renal disease, liver damage including cirrhosis, endocrine and adrenal gland issues, elevated stress hormones and hyponatremia". Patients with heart failure are recommended to restrict fluid intake down to 2 quarts per day.
Transurethral resection of the prostate (TURP) syndrome is a rare but potentially life-threatening complication of a transurethral resection of the prostate procedure. It occurs as a consequence of the absorption of the fluids used to irrigate the bladder during the operation into the prostatic venous sinuses. Symptoms and signs are varied and unpredictable, and result from fluid overload and disturbed electrolyte balance and hyponatremia. Treatment is largely supportive and relies on removal of the underlying cause, and organ and physiological support. Pre-operative prevention strategies are extremely important.
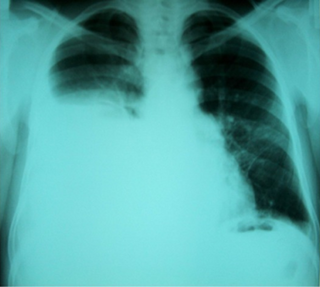
Hepatic hydrothorax is a rare form of pleural effusion that occurs in people with liver cirrhosis. It is defined as an effusion of over 500 mL in people with liver cirrhosis that is not caused by heart, lung, or pleural disease. It is found in 5–10% of people with liver cirrhosis and 2–3% of people with pleural effusions. In cases of decompensated liver cirrhosis, prevalence rises significantly up to 90%. Over 85% of cases occurring on the right, 13% on the left, and 2% on both. Although it is most common in people with severe ascites, it can also occur in people with mild or no ascites. Symptoms are not specific and mostly involve the respiratory system.