Dermatitis is a term used for different types of skin inflammation, typically characterized by itchiness, redness and a rash. In cases of short duration, there may be small blisters, while in long-term cases the skin may become thickened. The area of skin involved can vary from small to covering the entire body. Dermatitis is also called eczema but the same term is often used for the most common type of skin inflammation, atopic dermatitis.
An allergen is an otherwise harmless substance that triggers an allergic reaction in sensitive individuals by stimulating an immune response.

Eosinophilia is a condition in which the eosinophil count in the peripheral blood exceeds 5×108/L (500/μL). Hypereosinophilia is an elevation in an individual's circulating blood eosinophil count above 1.5 × 109/L (i.e. 1,500/μL). The hypereosinophilic syndrome is a sustained elevation in this count above 1.5 × 109/L (i.e. 1,500/μL) that is also associated with evidence of eosinophil-based tissue injury.

Ichthyosis vulgaris is a skin disorder causing dry, scaly skin. It is the most common form, and one of the mildest forms, of ichthyosis, affecting around 1 in 250 people. For this reason it is known as common ichthyosis. It is usually an autosomal dominant inherited disease, although a rare non-heritable version called acquired ichthyosis exists.

Pimecrolimus is an immunosuppressant drug of the calcineurin inhibitor class used in the treatment of atopic dermatitis (eczema).

Keratin 2A also known as keratin 2E or keratin 2 is a protein that in humans is encoded by the KRT2A gene.

Atopy is the tendency to produce an exaggerated immunoglobulin E (IgE) immune response to otherwise harmless substances in the environment. Allergic diseases are clinical manifestations of such inappropriate, atopic responses.

Atopic dermatitis (AD), also known as atopic eczema, is a long-term type of inflammation of the skin. AD is also often called simply eczema but the same term is also used to refer to dermatitis, the larger group of skin conditions. AD results in itchy, red, swollen, and cracked skin. Clear fluid may come from the affected areas, which can thicken over time.

Filaggrin is a filament-associated protein that binds to keratin fibers in epithelial cells. Ten to twelve filaggrin units are post-translationally hydrolyzed from a large profilaggrin precursor protein during terminal differentiation of epidermal cells. In humans, profilaggrin is encoded by the FLG gene, which is part of the S100 fused-type protein (SFTP) family within the epidermal differentiation complex on chromosome 1q21. In cetaceans and sirenians, the FLG family has lost its function, with the curious exception of manatees in the latter clade: manatees still retain some functional FLG genes.
Desmoglein-1 is a protein that in humans is encoded by the DSG1 gene. Desmoglein-1 is expressed everywhere in the skin epidermis, but mainly it is expressed in the superficial upper layers of the skin epidermis.

Urocanic acid is an intermediate in the catabolism of L-histidine. The cis-urocanic acid isomer is rare.

Netherton syndrome is a severe, autosomal recessive form of ichthyosis associated with mutations in the SPINK5 gene. It is named after Earl W. Netherton (1910–1985), an American dermatologist who discovered it in 1958.

The neuropeptide S receptor (NPSR) is a member of the G-protein coupled receptor superfamily of integral membrane proteins which binds neuropeptide S (NPS). It was formerly an orphan receptor, GPR154, until the discovery of neuropeptide S as the endogenous ligand. Increased expression of this gene in ciliated cells of the respiratory epithelium and in bronchial smooth muscle cells is associated with asthma. This gene is a member of the G protein-coupled receptor 1 family and encodes a plasma membrane protein. Mutations in this gene have also been associated with this disease.
Topical steroids are the topical forms of corticosteroids. Topical steroids are the most commonly prescribed topical medications for the treatment of rash and eczema. Topical steroids have anti-inflammatory properties and are classified based on their skin vasoconstrictive abilities. There are numerous topical steroid products. All the preparations in each class have the same anti-inflammatory properties but essentially differ in base and price.
Trichorrhexis invaginata is a distinctive hair shaft abnormality that may occur sporadically, either in normal hair or with other hair shaft abnormalities, or regularly as a marker for Netherton syndrome. The primary defect appears to be abnormal keratinization of the hair shaft in the keratogenous zone, allowing for intussusception of the fully keratinized and hard distal shaft into the incompletely keratinized and soft proximal portion of the shaft.

Meesmann corneal dystrophy (MECD) is a rare hereditary autosomal dominant disease that is characterized as a type of corneal dystrophy and a keratin disease. MECD is characterized by the formation of microcysts in the outermost layer of the cornea, known as the anterior corneal epithelium. The anterior corneal epithelium also becomes fragile. This usually affects both eyes rather than a single eye and worsens over time. There are two phenotypes, Meesmann corneal dystrophy 1 (MECD1) and Meesmann corneal dystrophy 2 (MECD2), which affect the genes KRT3 and KRT12, respectively. A heterozygous mutation in either of these genes will lead to a single phenotype. Many with Meesmann corneal dystrophy are asymptomatic or experience mild symptoms.

Autoimmune polyendocrine syndrome type 1 (APS-1), is a subtype of autoimmune polyendocrine syndrome. It causes the dysfunction of multiple endocrine glands due to autoimmunity. It is a genetic disorder, inherited in autosomal recessive fashion due to a defect in the AIRE gene , which is located on chromosome 21 and normally confers immune tolerance.
Mast cell activation syndrome (MCAS) is a term referring to one of two types of mast cell activation disorder (MCAD); the other type is idiopathic MCAD. MCAS is an immunological condition in which mast cells inappropriately and excessively release chemical mediators, resulting in a range of chronic symptoms, sometimes including anaphylaxis or near-anaphylaxis attacks. Primary symptoms include cardiovascular, dermatological, gastrointestinal, neurological, and respiratory problems.
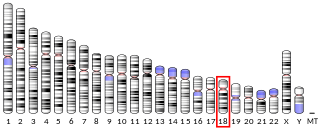
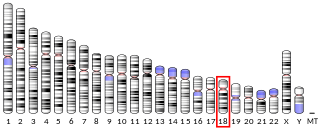
The epidermal differentiation complex (EDC) is a gene complex comprising over fifty genes encoding proteins involved in the terminal differentiation and cornification of keratinocytes, the primary cell type of the epidermis. In humans, the complex is located on a 1.9 Mbp stretch within chromosome 1q21. The proteins encoded by EDC genes are closely related in terms of function, and evolutionarily they belong to three distinct gene families: the cornified envelope precursor family, the S100 protein family and the S100 fused type protein (SFTP) family.

ORMDL sphingolipid biosynthesis regulator 3 is a protein that in humans is encoded by the ORMDL3 gene. Variants affecting the expression of this gene are associated with asthma in childhood. Transgenic mice which overexpress human ORMDL3 have increased levels of IgE. This correlated with increased numbers of macrophages, neutrophils, eosinophils, CD4+ and enhanced Th2 cytokine levels in the lung tissue.