Related Research Articles
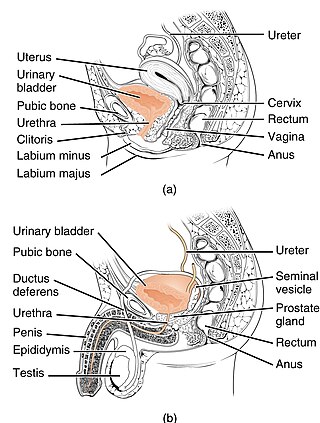
The urethra is a tube that connects the urinary bladder to the urinary meatus for the removal of urine from the body of both females and males. In human females and other primates, the urethra connects to the urinary meatus above the vagina, whereas in marsupials, the female's urethra empties into the urogenital sinus.

In mammals, the vagina is the elastic, muscular part of the female genital tract. In humans, it extends from the vestibule to the cervix. The outer vaginal opening is normally partly covered by a thin layer of mucosal tissue called the hymen. At the deep end, the cervix bulges into the vagina. The vagina allows for sexual intercourse and birth. It also channels menstrual flow, which occurs in humans and closely related primates as part of the menstrual cycle.

The perineum in humans is the space between the anus and scrotum in the male, or between the anus and the vulva in the female. The perineum is the region of the body between the pubic symphysis and the coccyx, including the perineal body and surrounding structures. There is some variability in how the boundaries are defined. The perineal raphe is visible and pronounced to varying degrees. The perineum is an erogenous zone.

The pudendal nerve is the main nerve of the perineum. It carries sensation from the external genitalia of both sexes and the skin around the anus and perineum, as well as the motor supply to various pelvic muscles, including the male or female external urethral sphincter and the external anal sphincter. If damaged, most commonly by childbirth, loss of sensation or fecal incontinence may result. The nerve may be temporarily anesthetized, called pudendal anesthesia or pudendal block.

The levator ani is a broad, thin muscle group, situated on either side of the pelvis. It is formed from three muscle components: the pubococcygeus, the iliococcygeus, and the puborectalis.

The coccyx, commonly referred to as the tailbone, is the final segment of the vertebral column in all apes, and analogous structures in certain other mammals such as horses. In tailless primates since Nacholapithecus, the coccyx is the remnant of a vestigial tail. In animals with bony tails, it is known as tailhead or dock, in bird anatomy as tailfan. It comprises three to five separate or fused coccygeal vertebrae below the sacrum, attached to the sacrum by a fibrocartilaginous joint, the sacrococcygeal symphysis, which permits limited movement between the sacrum and the coccyx.

Vaginismus is a condition in which involuntary muscle spasm interferes with vaginal intercourse or other penetration of the vagina. This often results in pain with attempts at sex. Often, it begins when vaginal intercourse is first attempted.
Dyspareunia is painful sexual intercourse due to medical or psychological causes. The term dyspareunia covers both female dyspareunia and male dyspareunia, but many discussions that use the term without further specification concern the female type, which is more common than the male type. In females, the pain can primarily be on the external surface of the genitalia, or deeper in the pelvis upon deep pressure against the cervix. Medically, dyspareunia is a pelvic floor dysfunction and is frequently underdiagnosed. It can affect a small portion of the vulva or vagina or be felt all over the surface. Understanding the duration, location, and nature of the pain is important in identifying the causes of the pain.

Kegel exercise, also known as pelvic-floor exercise, involves repeatedly contracting and relaxing the muscles that form part of the pelvic floor, now sometimes colloquially referred to as the "Kegel muscles". The exercise can be performed many times a day, for several minutes at a time but takes one to three months to begin to have an effect.

The pelvic floor or pelvic diaphragm is composed of muscle fibers of the levator ani, the coccygeus muscle, and associated connective tissue which span the area underneath the pelvis. The pelvic diaphragm is a muscular partition formed by the levatores ani and coccygei, with which may be included the parietal pelvic fascia on their upper and lower aspects. The pelvic floor separates the pelvic cavity above from the perineal region below. Both males and females have a pelvic floor. To accommodate the birth canal, a female's pelvic cavity is larger than a male's.

Pelvic floor dysfunction is a term used for a variety of disorders that occur when pelvic floor muscles and ligaments are impaired. The condition affects up to 50 percent of women who have given birth. Although this condition predominantly affects women, up to 16 percent of men are affected as well. Symptoms can include pelvic pain, pressure, pain during sex, urinary incontinence (UI), overactive bladder, bowel incontinence, incomplete emptying of feces, constipation, myofascial pelvic pain and pelvic organ prolapse. When pelvic organ prolapse occurs, there may be visible organ protrusion or a lump felt in the vagina or anus.

The cystocele, also known as a prolapsed bladder, is a medical condition in which a woman's bladder bulges into her vagina. Some may have no symptoms. Others may have trouble starting urination, urinary incontinence, or frequent urination. Complications may include recurrent urinary tract infections and urinary retention. Cystocele and a prolapsed urethra often occur together and is called a cystourethrocele. Cystocele can negatively affect quality of life.

The coccygeus muscle or ischiococcygeus is a muscle of the pelvic floor, located posterior to levator ani and anterior to the sacrospinous ligament.

Perineal hernia is a hernia involving the perineum. The hernia may contain fluid, fat, any part of the intestine, the rectum, or the bladder. It is known to occur in humans, dogs, and other mammals, and often appears as a sudden swelling to one side of the anus.

Uterine prolapse is a form of pelvic organ prolapse in which the uterus and a portion of the upper vagina protrude into the vaginal canal and, in severe cases, through the opening of the vagina. It is most often caused by injury or damage to structures that hold the uterus in place within the pelvic cavity. Symptoms may include vaginal fullness, pain with sexual intercourse, difficulty urinating, and urinary incontinence. Risk factors include older age, pregnancy, vaginal childbirth, obesity, chronic constipation, and chronic cough. Prevalence, based on physical exam alone, is estimated to be approximately 14%.

The pelvic fasciae are the fascia of the pelvis and can be divided into:

The external sphincter muscle of female urethra is a muscle which controls urination in females. The muscle fibers arise on either side from the margin of the inferior ramus of the pubis. They are directed across the pubic arch in front of the urethra, and pass around it to blend with the muscular fibers of the opposite side, between the urethra and vagina.

The rectococcygeal muscles are two bands of smooth muscle tissue arising from the 2nd and 3rd coccygeal vertebrae, and passing downward and forward to blend with the rectal longitudinal smooth muscle fibers on the posterior wall of the anal canal.

The vaginal support structures are those muscles, bones, ligaments, tendons, membranes and fascia, of the pelvic floor that maintain the position of the vagina within the pelvic cavity and allow the normal functioning of the vagina and other reproductive structures in the female. Defects or injuries to these support structures in the pelvic floor leads to pelvic organ prolapse. Anatomical and congenital variations of vaginal support structures can predispose a woman to further dysfunction and prolapse later in life. The urethra is part of the anterior wall of the vagina and damage to the support structures there can lead to incontinence and urinary retention.
Vaginal rugae are structures of the vagina that are transverse ridges formed out of the supporting tissues and vaginal epithelium in females. Some conditions can cause the disappearance of vaginal rugae and are usually associated with childbirth and prolapse of pelvic structures. The rugae contribute to the resiliency and elasticity of the vagina and its ability to distend and return to its previous state. These structures not only allow expansions and an increase in surface area of the vaginal epithelium, they provide the space necessary for the vaginal microbiota. The shape and structure of the rugae are supported and maintained by the lamina propria of the vagina and the anterior and posterior rugae.
References
- ↑ "Pubovaginalis muscle". www.pelviperineology.org. Retrieved 2018-02-07.
- ↑ "the definition of pubovaginal muscle". Dictionary.com. Retrieved 2018-02-07.
- ↑ "pubovaginal muscle". TheFreeDictionary.com. Retrieved 2018-02-07.
- ↑ "pubovaginal muscle". Academic Dictionaries and Encyclopedias. Retrieved 2018-02-07.
- ↑ Stoker, Jaap; Taylor, Stuart A.; Delancey, John O. L. (2010-03-28). Imaging Pelvic Floor Disorders. Springer Science & Business Media. ISBN 9783540719687.
- ↑ Craft, T. M.; Parr, M. J. A.; Nolan, Jerry P. (2004-11-10). Key Topics in Critical Care, Second Edition. CRC Press. ISBN 9781841843582.
- ↑ Ashton-Miller, James A.; DeLANCEY, John O. L. (2007-04-01). "Functional Anatomy of the Female Pelvic Floor" (PDF). Annals of the New York Academy of Sciences. 1101 (1): 266–296. Bibcode:2007NYASA1101..266A. doi:10.1196/annals.1389.034. hdl: 2027.42/72597 . ISSN 1749-6632. PMID 17416924. S2CID 6310287.
- ↑ Grim, Miloš (2017). "Clinical topographic anatomy" (PDF). Institute of Anatomy, First Faculty of Medicine, Charles University.
- 1 2 Nyangoh Timoh, Krystel; Moszkowicz, David; Zaitouna, Mazen; Lebacle, Cedric; Martinovic, Jelena; Diallo, Djibril; Creze, Maud; Lavoue, Vincent; Darai, Emile (2018). "Detailed muscular structure and neural control anatomy of the levator ani muscle: a study based on female human fetuses". American Journal of Obstetrics and Gynecology. 218 (1): 121.e1–121.e12. doi:10.1016/j.ajog.2017.09.021. PMID 28988909. S2CID 29761046.
- ↑ Hoyte, Lennox; Damaser, Margot (2016-03-01). Biomechanics of the Female Pelvic Floor. Academic Press. ISBN 9780128032299.
- ↑ Progressive Medicine. 1912.