Related Research Articles

Systemic scleroderma, or systemic sclerosis, is an autoimmune rheumatic disease characterised by excessive production and accumulation of collagen, called fibrosis, in the skin and internal organs and by injuries to small arteries. There are two major subgroups of systemic sclerosis based on the extent of skin involvement: limited and diffuse. The limited form affects areas below, but not above, the elbows and knees with or without involvement of the face. The diffuse form also affects the skin above the elbows and knees and can also spread to the torso. Visceral organs, including the kidneys, heart, lungs, and gastrointestinal tract can also be affected by the fibrotic process. Prognosis is determined by the form of the disease and the extent of visceral involvement. Patients with limited systemic sclerosis have a better prognosis than those with the diffuse form. Death is most often caused by lung, heart, and kidney involvement. The risk of cancer is increased slightly.

Antinuclear antibodies are autoantibodies that bind to contents of the cell nucleus. In normal individuals, the immune system produces antibodies to foreign proteins (antigens) but not to human proteins (autoantigens). In some cases, antibodies to human antigens are produced.
Rheumatism or rheumatic disorders are conditions causing chronic, often intermittent pain affecting the joints or connective tissue. Rheumatism does not designate any specific disorder, but covers at least 200 different conditions, including arthritis and "non-articular rheumatism", also known as "regional pain syndrome" or "soft tissue rheumatism". There is a close overlap between the term soft tissue disorder and rheumatism. Sometimes the term "soft tissue rheumatic disorders" is used to describe these conditions.

Raynaud syndrome, also known as Raynaud's phenomenon, eponymously named after the physician, Auguste Gabriel Maurice Raynaud, who first described it in his doctoral thesis in 1862, is a medical condition in which the spasm of small arteries causes episodes of reduced blood flow to end arterioles. Typically, the fingers, and less commonly the toes, are involved. Rarely, the nose, ears, or lips are affected. The episodes classically result in the affected part turning white and then blue. Often, numbness or pain occurs. As blood flow returns, the area turns red and burns. The episodes typically last minutes, but can last several hours.

Juvenile dermatomyositis (JDM) is an idiopathic inflammatory myopathy (IMM) of presumed autoimmune dysfunction resulting in muscle weakness among other complications. It manifests itself in children; it is the pediatric counterpart of dermatomyositis. In JDM, the body's immune system attacks blood vessels throughout the body, causing inflammation called vasculitis. In the United States, the incidence rate of JDMS is approximately 2-3 cases per million children per year. The UK incidence is believed to be between 2-3 per million children per year, with some difference between ethnic groups. The sex ratio is approximately 2:1. Other Idiopathic inflammatory myopathies include; juvenile polymyositis (PM), which is rare and not as common in children as in adults.

Dermatomyositis (DM) is a long-term inflammatory disorder which affects skin and the muscles. Its symptoms are generally a skin rash and worsening muscle weakness over time. These may occur suddenly or develop over months. Other symptoms may include weight loss, fever, lung inflammation, or light sensitivity. Complications may include calcium deposits in muscles or skin.

CREST syndrome, also known as the limited cutaneous form of systemic sclerosis (lcSSc), is a multisystem connective tissue disorder. The acronym "CREST" refers to the five main features: calcinosis, Raynaud's phenomenon, esophageal dysmotility, sclerodactyly, and telangiectasia.

Polymyositis (PM) is a type of chronic inflammation of the muscles related to dermatomyositis and inclusion body myositis. Its name means "inflammation of many muscles". The inflammation of polymyositis is mainly found in the endomysial layer of skeletal muscle, whereas dermatomyositis is characterized primarily by inflammation of the perimysial layer of skeletal muscles.
A connective tissue disease (collagenosis) is any disease that has the connective tissues of the body as a target of pathology. Connective tissue is any type of biological tissue with an extensive extracellular matrix that supports, binds together, and protects organs. These tissues form a framework, or matrix, for the body, and are composed of two major structural protein molecules: collagen and elastin. There are many different types of collagen protein in each of the body's tissues. Elastin has the capability of stretching and returning to its original length—like a spring or rubber band. Elastin is the major component of ligaments and skin. In patients with connective tissue disease, it is common for collagen and elastin to become injured by inflammation (ICT). Many connective tissue diseases feature abnormal immune system activity with inflammation in tissues as a result of an immune system that is directed against one's own body tissues (autoimmunity).

Morphea, is a form of scleroderma that involves isolated patches of hardened skin on the face, hands, and feet, or anywhere else on the body, with no internal organ involvement.
Extractable Nuclear Antigens (ENAs) are over 100 different soluble cytoplasmic and nuclear antigens. They are known as “extractable” because they can be removed from cell nuclei using saline and represent six main proteins: Ro, La, Sm, RNP, Scl-70, Jo1. Most ENAs are part of spliceosomes or nucleosomes complexes and are a type of small nuclear ribonucleoprotein (snRNPS). The location in the nucleus and association with spliceosomes or nucleosomes results in these ENAs being associated with additional RNA and proteins such as polymerases. This quality of ENAs often makes it difficult to purify and quantify their presence for clinical use.
Mixed connective tissue disease commonly abbreviated as MCTD, is an autoimmune disease characterized by the presence of elevated blood levels of a specific autoantibody, now called anti-U1 ribonucleoprotein (RNP) together with a mix of symptoms of systemic lupus erythematosus (SLE), scleroderma, and polymyositis. The idea behind the "mixed" disease is that this specific autoantibody is also present in other autoimmune diseases such as systemic lupus erythematosus, polymyositis, scleroderma, etc. MCTD was characterized as an individual disease in 1972 by Sharp et al., and the term was introduced by Leroy in 1980.
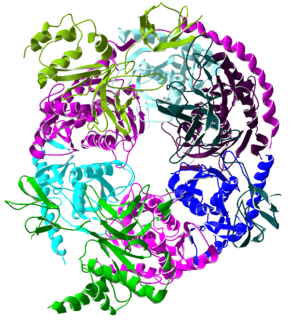
The exosome complex is a multi-protein intracellular complex capable of degrading various types of RNA molecules. Exosome complexes are found in both eukaryotic cells and archaea, while in bacteria a simpler complex called the degradosome carries out similar functions.
An overlap syndrome is a medical condition which shares features of at least two more widely recognised disorders. Examples of overlap syndromes can be found in many medical specialties such as overlapping connective tissue disorders in rheumatology, and overlapping genetic disorders in cardiology.
Anti-topoisomerase antibodies (ATA) are autoantibodies directed against topoisomerase and found in several diseases, most importantly scleroderma. Diseases with ATA are autoimmune disease because they react with self-proteins. They are also referred to as anti-DNA topoisomerase I antibody.

Scleroderma is a group of autoimmune diseases that may result in changes to the skin, blood vessels, muscles, and internal organs. The disease can be either localized to the skin or involve other organs, as well. Symptoms may include areas of thickened skin, stiffness, feeling tired, and poor blood flow to the fingers or toes with cold exposure. One form of the condition, known as CREST syndrome, classically results in calcium deposits, Raynaud's syndrome, esophageal problems, thickening of the skin of the fingers and toes, and areas of small, dilated blood vessels.
Cryofibrinogenemia refers to a condition classified as a fibrinogen disorder in which the chilling of an individual's blood plasma from the normal body temperature of 37 °C to the near-freezing temperature of 4 °C causes the reversible precipitation of a complex containing fibrinogen, fibrin, fibronectin, and, occasionally, small amounts of fibrin split products, albumin, immunoglobulins and other plasma proteins. Returning this plasma to 37 °C resolubilizes the precipitate.
Undifferentiated connective tissue disease (UCTD) is a disease in which the body mistakenly attacks its own tissues. It is diagnosed when there is evidence of an existing autoimmune condition which does not meet the criteria for any specific autoimmune disease, such as systemic lupus erythematosus or scleroderma. Latent lupus and incomplete lupus are alternative terms that have been used to describe this condition.

Anti-SSA autoantibodies are a type of anti-nuclear autoantibodies that are associated with many autoimmune diseases, such as systemic lupus erythematosus (SLE), SS/SLE overlap syndrome, subacute cutaneous lupus erythematosus (SCLE), neonatal lupus and primary biliary cirrhosis. They are often present in Sjögren's syndrome (SS). Additionally, Anti-Ro/SSA can be found in other autoimmune diseases such as systemic sclerosis (SSc), polymyositis/dermatomyositis (PM/DM), rheumatoid arthritis (RA), and mixed connective tissue disease (MCTD), and are also associated with heart arrhythmia.
Anti-synthetase syndrome is an autoimmune disease associated with interstitial lung disease, dermatomyositis, and polymyositis.
References
- ↑ Jablonska S.; Blaszczyk M. (1999). "Scleroderma overlap syndromes". Adv Exp Med Biol. Advances in Experimental Medicine and Biology. 455: 85–92. doi:10.1007/978-1-4615-4857-7_12. ISBN 978-1-4613-7203-5. PMID 10599327.
- ↑ Mahler, M.; Raijmakers R. (2007). "Novel aspects of autoantibodies to the PM/Scl complex: Clinical, genetic and diagnostic insights". Autoimmunity Reviews. 6 (7): 432–7. doi:10.1016/j.autrev.2007.01.013. PMID 17643929.
- ↑ Jablonska S.; Blaszczyk M. (1998). "Scleromyositis: a scleroderma/polymyositis overlap syndrome". Clinical Rheumatology. 17 (6): 465–7. doi:10.1007/BF01451281. PMID 9890673. S2CID 39237322.
- ↑ Vandergheynst F, Ocmant A, Sordet C, Humbel RL, Goetz J, Roufosse F, Cogan E, Sibilia J (2006). "Anti-pm/scl antibodies in connective tissue disease: Clinical and biological assessment of 14 patients". Clinical and Experimental Rheumatology. 24 (2): 129–33. PMID 16762146.
- ↑ Saw, Jacqui; Leong, Wai; John, Mina; Nolan, David; O'Connor, Kevin (2014). "70: Vitamin R therapy in scleromyositis: A novel approach for a rare disorder". Journal of Clinical Neuroscience. 21 (11): 2054–5. doi:10.1016/j.jocn.2014.06.084. S2CID 54300075.