 | |
 | |
| Clinical data | |
|---|---|
| AHFS/Drugs.com | Micromedex Detailed Consumer Information |
| MedlinePlus | a600027 |
| ATC code | |
| Pharmacokinetic data | |
| Elimination half-life | 1.5 days |
| Identifiers | |
| |
| CAS Number | |
| PubChem CID | |
| IUPHAR/BPS | |
| DrugBank | |
| ChemSpider | |
| UNII | |
| KEGG | |
| ChEBI | |
| ChEMBL | |
| CompTox Dashboard (EPA) | |
| ECHA InfoCard | 100.000.220 |
| Chemical and physical data | |
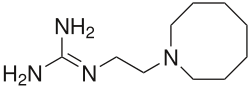
| Formula | C10H22N4 |
| Molar mass | 198.314 g·mol−1 |
| 3D model (JSmol) | |
| |
| |
| | |
Guanethidine is an antihypertensive drug that reduces the release of catecholamines, such as norepinephrine. Guanethidine is transported across the sympathetic nerve membrane by the same mechanism that transports norepinephrine itself (NET, uptake 1), and uptake is essential for the drug's action. Once guanethidine has entered the nerve, it is concentrated in transmitter vesicles, where it replaces norepinephrine. It may also inhibit the release of granules by decreasing norepinephrine.