Beta blockers, also spelled β-blockers, are a class of medications that are predominantly used to manage abnormal heart rhythms (arrhythmia), and to protect the heart from a second heart attack after a first heart attack. They are also widely used to treat high blood pressure, although they are no longer the first choice for initial treatment of most people.

Phenylephrine, sold under the brand names Neosynephrine and Sudafed PE among others, is a medication used as a decongestant for uncomplicated nasal congestion in the form of a nasal spray or oral tablet, to dilate the pupil, to increase blood pressure given intravenously in cases of low blood pressure, and to relieve hemorrhoids as a suppository. It can also be applied to the skin.
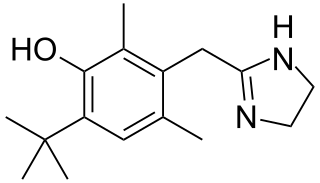
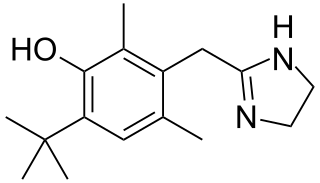
Oxymetazoline, sold under the brand name Afrin among others, is a topical decongestant and vasoconstrictor medication. It is available over-the-counter as a nasal spray to treat nasal congestion and nosebleeds, as eye drops to treat eye redness due to minor irritation, and as a prescription topical cream to treat persistent facial redness due to rosacea in adults. Its effects begin within minutes and last for up to six hours. Intranasal use for longer than three to five days may cause congestion to recur or worsen, resulting in physical dependence.
An adrenergic agonist is a drug that stimulates a response from the adrenergic receptors. The five main categories of adrenergic receptors are: α1, α2, β1, β2, and β3, although there are more subtypes, and agonists vary in specificity between these receptors, and may be classified respectively. However, there are also other mechanisms of adrenergic agonism. Epinephrine and norepinephrine are endogenous and broad-spectrum. More selective agonists are more useful in pharmacology.
Labetalol is a medication used to treat high blood pressure and in long term management of angina. This includes essential hypertension, hypertensive emergencies, and hypertension of pregnancy. In essential hypertension it is generally less preferred than a number of other blood pressure medications. It can be given by mouth or by injection into a vein.
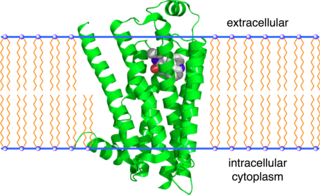
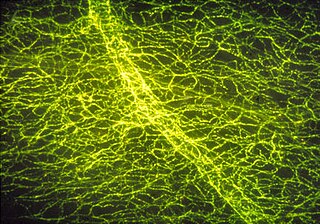
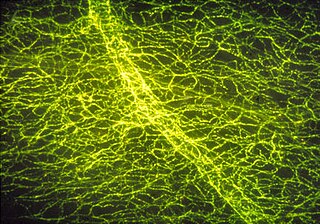
alpha-1 (α1) adrenergic receptors are G protein-coupled receptors (GPCRs) associated with the Gq heterotrimeric G protein. α1-adrenergic receptors are subdivided into three highly homologous subtypes, i.e., α1A-, α1B-, and α1D-adrenergic receptor subtypes. There is no α1C receptor. At one time, there was a subtype known as α1C, but it was found to be identical to the previously discovered α1A receptor subtype. To avoid confusion, naming was continued with the letter D. Catecholamines like norepinephrine (noradrenaline) and epinephrine (adrenaline) signal through the α1-adrenergic receptors in the central and peripheral nervous systems. The crystal structure of the α1B-adrenergic receptor subtype has been determined in complex with the inverse agonist (+)-cyclazosin.

The alpha-2 (α2) adrenergic receptor is a G protein-coupled receptor (GPCR) associated with the Gi heterotrimeric G-protein. It consists of three highly homologous subtypes, including α2A-, α2B-, and α2C-adrenergic. Some species other than humans express a fourth α2D-adrenergic receptor as well. Catecholamines like norepinephrine (noradrenaline) and epinephrine (adrenaline) signal through the α2-adrenergic receptor in the central and peripheral nervous systems.
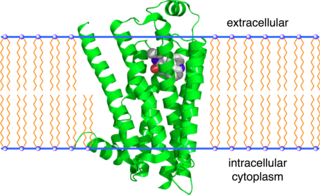
The beta-2 adrenergic receptor, also known as ADRB2, is a cell membrane-spanning beta-adrenergic receptor that binds epinephrine (adrenaline), a hormone and neurotransmitter whose signaling, via adenylate cyclase stimulation through trimeric Gs proteins, increases cAMP, and, via downstream L-type calcium channel interaction, mediates physiologic responses such as smooth muscle relaxation and bronchodilation.

Alpha-adrenergic agonists are a class of sympathomimetic agents that selectively stimulates alpha adrenergic receptors. The alpha-adrenergic receptor has two subclasses α1 and α2. Alpha 2 receptors are associated with sympatholytic properties. Alpha-adrenergic agonists have the opposite function of alpha blockers. Alpha adrenoreceptor ligands mimic the action of epinephrine and norepinephrine signaling in the heart, smooth muscle and central nervous system, with norepinephrine being the highest affinity. The activation of α1 stimulates the membrane bound enzyme phospholipase C, and activation of α2 inhibits the enzyme adenylate cyclase. Inactivation of adenylate cyclase in turn leads to the inactivation of the secondary messenger cyclic adenosine monophosphate and induces smooth muscle and blood vessel constriction.

Cirazoline is a full agonist at the α1A adrenergic receptor, a partial agonist at both the α1B and α1D adrenergic receptors, and a nonselective antagonist to the α2 adrenergic receptor. It is believed that this combination of properties could make cirazoline an effective vasoconstricting agent.

An adrenergic antagonist is a drug that inhibits the function of adrenergic receptors. There are five adrenergic receptors, which are divided into two groups. The first group of receptors are the beta (β) adrenergic receptors. There are β1, β2, and β3 receptors. The second group contains the alpha (α) adrenoreceptors. There are only α1 and α2 receptors. Adrenergic receptors are located near the heart, kidneys, lungs, and gastrointestinal tract. There are also α-adreno receptors that are located on vascular smooth muscle.
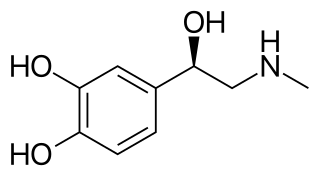
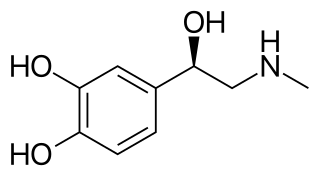
Adrenaline, also known as epinephrine, is a hormone and medication which is involved in regulating visceral functions. It appears as a white microcrystalline granule. Adrenaline is normally produced by the adrenal glands and by a small number of neurons in the medulla oblongata. It plays an essential role in the fight-or-flight response by increasing blood flow to muscles, heart output by acting on the SA node, pupil dilation response, and blood sugar level. It does this by binding to alpha and beta receptors. It is found in many animals, including humans, and some single-celled organisms. It has also been isolated from the plant Scoparia dulcis found in Northern Vietnam.

Alpha blockers, also known as α-blockers or α-adrenoreceptor antagonists, are a class of pharmacological agents that act as antagonists on α-adrenergic receptors (α-adrenoceptors).
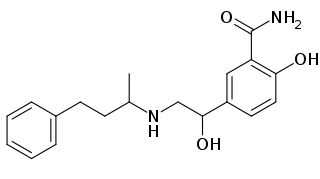
Beta adrenergic agonists or beta agonists are medications that relax muscles of the airways, causing widening of the airways and resulting in easier breathing. They are a class of sympathomimetic agents, each acting upon the beta adrenoceptors. In general, pure beta-adrenergic agonists have the opposite function of beta blockers: beta-adrenoreceptor agonist ligands mimic the actions of both epinephrine- and norepinephrine- signaling, in the heart and lungs, and in smooth muscle tissue; epinephrine expresses the higher affinity. The activation of β1, β2 and β3 activates the enzyme, adenylate cyclase. This, in turn, leads to the activation of the secondary messenger cyclic adenosine monophosphate (cAMP); cAMP then activates protein kinase A (PKA) which phosphorylates target proteins, ultimately inducing smooth muscle relaxation and contraction of the cardiac tissue.
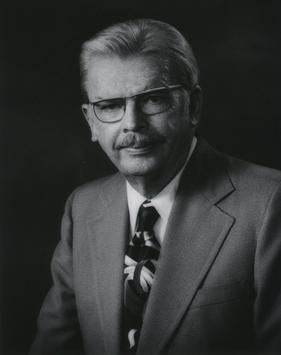
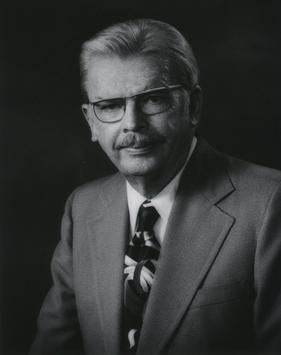
Raymond Perry Ahlquist was an American pharmacist and pharmacologist. He published seminal work in 1948 that divided adrenoceptors into α- and β-adrenoceptor subtypes. This discovery explained the activity of several existing drugs and also laid the groundwork for new drugs including the widely prescribed beta blockers.
The catecholamines are a group of neurotransmitters composed of the endogenous substances dopamine, noradrenaline (norepinephrine), and adrenaline (epinephrine), as well as numerous artificially synthesized compounds such as isoprenaline - an anti-bradycardiac medication. Their investigation constitutes a major chapter in the history of physiology, biochemistry, and pharmacology. Adrenaline was the first hormone extracted from an endocrine gland and obtained in pure form, before the word hormone was coined. Adrenaline was also the first hormone whose structure and biosynthesis was discovered. Second to acetylcholine, adrenaline and noradrenaline were some of the first neurotransmitters discovered, and the first intercellular biochemical signals to be found in intracellular vesicles. The β-adrenoceptor gene was the first G protein-coupled receptor to be cloned.
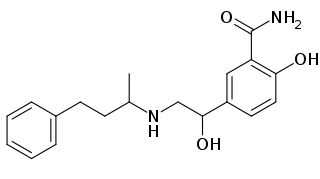
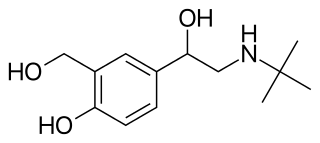
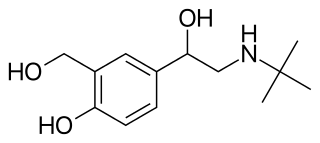
β2-adrenoceptor agonists are a group of drugs that act selectively on β2-receptors in the lungs causing bronchodilation. β2-agonists are used to treat asthma and COPD, diseases that cause obstruction in the airways. Prior to their discovery, the non-selective beta-agonist isoprenaline was used. The aim of the drug development through the years has been to minimise side effects, achieve selectivity and longer duration of action. The mechanism of action is well understood and has facilitated the development. The structure of the binding site and the nature of the binding is also well known, as is the structure activity relationship.
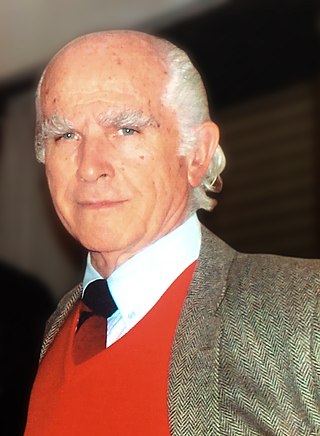
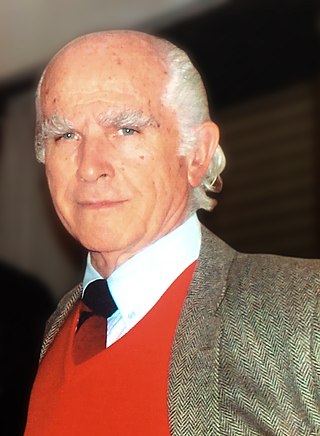
Serafim Guimarães, full name Serafim Correia Pinto Guimarães, is a Portuguese physician and pharmacologist. With his colleague Walter Osswald he made the Department of Pharmacology, Medical Faculty of the University of Porto, a center of research on catecholamines and the sympathetic nervous system, especially their relation to blood vessels.
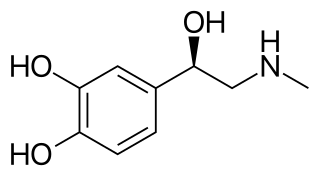
Epinephrine, also known as adrenaline, is a medication and hormone. As a medication, it is used to treat several conditions, including anaphylaxis, cardiac arrest, asthma, and superficial bleeding. Inhaled epinephrine may be used to improve the symptoms of croup. It may also be used for asthma when other treatments are not effective. It is given intravenously, by injection into a muscle, by inhalation, or by injection just under the skin.
Autonomic drugs are substances that can either inhibit or enhance the functions of the parasympathetic and sympathetic nervous systems. This type of drug can be used to treat a wide range of diseases an disorders, including glaucoma, asthma, and disorders of the urinary, gastrointestinal and circulatory systems.