Ligand binding and signal transduction
Upon initial binding to the LRR region of FSHR, FSH reshapes its conformation to form a new pocket. FSHR then inserts its sulfotyrosine from the hinge loop into the pockets and activates the 7-helical transmembrane domain. [6] This event leads to a transduction of the signal that activates the Gs protein that is bound to the receptor internally. With FSH attached, the receptor shifts conformation and, thus, mechanically activates the G protein, which detaches from the receptor and activates the cAMP system. [9] [10]
It is believed that a receptor molecule exists in a conformational equilibrium between active and inactive states. The binding of FSH to the receptor shifts the equilibrium between active and inactive receptors. FSH and FSH-agonists shift the equilibrium in favor of active states; FSH antagonists shift the equilibrium in favor of inactive states.
Phosphorylation by cAMP-dependent protein kinases
Cyclic AMP-dependent protein kinases (protein kinase A) are activated by the signal chain coming from the Gs protein (that was activated by the FSH-receptor) via adenylate cyclase and cyclic AMP (cAMP). [9] [10]
These protein kinases are present as tetramers with two regulatory units and two catalytic units. Upon binding of cAMP to the regulatory units, the catalytic units are released and initiate the phosphorylation of proteins, leading to the physiologic action. The cyclic AMP-regulatory dimers are degraded by phosphodiesterase and release 5'AMP. DNA in the cell nucleus binds to phosphorylated proteins through the cyclic AMP response element (CRE), which results in the activation of genes. [5]
The signal is amplified by the involvement of cAMP and the resulting phosphorylation. The process is modified by prostaglandins. Other cellular regulators are participate are the intracellular calcium concentration modified by phospholipase, nitric acid, and other growth factors.
The FSH receptor can also activate the extracellular signal-regulated kinases (ERK). [11] In a feedback mechanism, these activated kinases phosphorylate the receptor.
Action
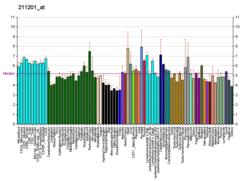
In the ovary, the FSH receptor is necessary for follicular development and expressed on the granulosa cells. [5]
In the male, the FSH receptor has been identified on the Sertoli cells that are critical for spermatogenesis. [12]
The FSHR is expressed during the luteal phase in the secretory endometrium of the uterus. [13]
FSH receptor is selectively expressed on the surface of the blood vessels of a wide range of carcinogenic tumors. [14]
FSH abnormalities
Some patients with ovarian hyperstimulation syndrome may have mutations in the gene for FSHR, making them more sensitive to gonadotropin stimulation. [16]
Women with 46 XX gonadal dysgenesis experience primary amenorrhea with hypergonadotropic hypogonadism. There are forms of 46 xx gonadal dysgenesis wherein abnormalities in the FSH-receptor have been reported and are thought to be the cause of the hypogonadism. [17]
Polymorphism may affect FSH receptor populations and lead to poorer responses in infertile women receiving FSH medication for IVF. [18]
Alternative splicing of the FSHR gene may be implicated in subfertility in males [19]
This page is based on this
Wikipedia article Text is available under the
CC BY-SA 4.0 license; additional terms may apply.
Images, videos and audio are available under their respective licenses.