 | |
 | |
| Clinical data | |
|---|---|
| Trade names | Lupron, Eligard, Lucrin, Lupaneta, others |
| Other names | leuprolide, leuprolidine, A-43818, Abbott-43818, DC-2-269, TAP-144 |
| AHFS/Drugs.com | Monograph |
| MedlinePlus | a685040 |
| License data |
|
| Pregnancy category |
|
| Routes of administration | implant, subcutaneous, intramuscular |
| Drug class | GnRH analogue; GnRH agonist; Antigonadotropin |
| ATC code | |
| Legal status | |
| Legal status | |
| Pharmacokinetic data | |
| Elimination half-life | 3 hours |
| Excretion | Kidney |
| Identifiers | |
| |
| CAS Number | |
| PubChem CID | |
| IUPHAR/BPS | |
| DrugBank | |
| ChemSpider | |
| UNII | |
| KEGG | |
| ChEMBL | |
| CompTox Dashboard (EPA) | |
| ECHA InfoCard | 100.161.466 |
| Chemical and physical data | |
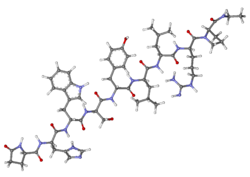
| Formula | C59H84N16O12 |
| Molar mass | 1209.421 g·mol−1 |
| 3D model (JSmol) | |
| |
| |
| | |
Leuprorelin, also known as leuprolide, is a manufactured version of a hormone used to treat prostate cancer, breast cancer, endometriosis, uterine fibroids, for early puberty, as part of transgender hormone therapy, or to perform chemical castration of violent sex offenders. [10] [11] [12] It is given by injection into a muscle or under the skin. [10]
Contents
- Medical uses
- Side effects
- Lupron "flare"
- Pharmacology
- Mechanism of action
- Available forms
- Chemistry
- History
- Approvals
- Society and culture
- Legal status
- Names
- Legal history
- Research
- Veterinary use
- References
- Further reading
Leuprorelin is in the gonadotropin-releasing hormone (GnRH) analogue family of medications. [10] It works by decreasing gonadotropins, thereby decreasing testosterone and estradiol. [10] Common side effects include hot flashes, unstable mood, trouble sleeping, headaches, and pain at the site of injection. [10] Other side effects may include high blood sugar, allergic reactions, and problems with the pituitary gland. [10] Use during pregnancy may harm foetal development. [10]
Leuprorelin was patented in 1973 and approved for medical use in the United States in 1985. [10] [13] It is on the World Health Organization's List of Essential Medicines. [11] It is sold under the brand name Lupron, among others. [10]