| Ischemic optic neuropathy | |
|---|---|
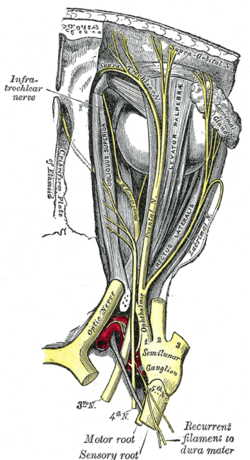 | |
| Optic nerve | |
| Specialty | Ophthalmology |
Ischemic optic neuropathy (ION) is the loss of structure and function of a portion of the optic nerve due to obstruction of blood flow to the nerve (i.e. ischemia). Ischemic forms of optic neuropathy are typically classified as either anterior ischemic optic neuropathy or posterior ischemic optic neuropathy according to the part of the optic nerve that is affected. People affected will often complain of a loss of visual acuity and a visual field, the latter of which is usually in the superior or inferior field. [1]
Contents
When ION occurs in patients below the age of 50 years old, other causes should be considered, such as juvenile diabetes mellitus, antiphospholipid antibody-associated clotting disorders, collagen-vascular disease, and migraines. Rarely, complications of intraocular surgery or acute blood loss may cause an ischemic event in the optic nerve. [2]