| Nerve fiber layer | |
|---|---|
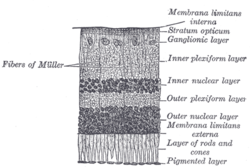 Section of retina. (Stratum opticum labeled at right, second from the top.) | |
 Plan of retinal neurons. (Stratum opticum labeled at left, second from the top.) | |
| Details | |
| Identifiers | |
| Latin | stratum neurofibrarum retinae |
| TA | A15.2.04.017 |
| FMA | 58688 |
| Anatomical terminology | |
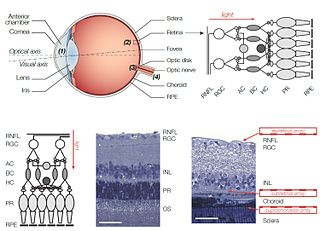
The retinal nerve fiber layer (nerve fiber layer, stratum opticum, RNFL) is formed by the expansion of the fibers of the optic nerve; it is thickest near the optic disc, gradually diminishing toward the ora serrata.

The retina is the innermost, light-sensitive layer of tissue of the eye of most vertebrates and some molluscs. The optics of the eye create a focused two-dimensional image of the visual world on the retina, which translates that image into electrical neural impulses to the brain to create visual perception, the retina serving a function analogous to that of the film or image sensor in a camera.
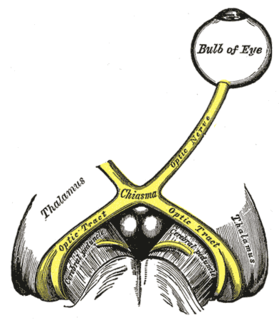
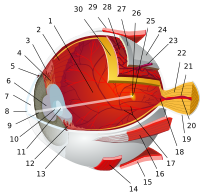
The optic nerve, also known as cranial nerve II, or simply as CN II, is a paired nerve that transmits visual information from the retina to the brain. In humans, the optic nerve is derived from optic stalks during the seventh week of development and is composed of retinal ganglion cell axons and glial cells; it extends from the optic disc to the optic chiasma and continues as the optic tract to the lateral geniculate nucleus, pretectal nuclei, and superior colliculus.

The optic disc or optic nerve head is the point of exit for ganglion cell axons leaving the eye. Because there are no rods or cones overlying the optic disc, it corresponds to a small blind spot in each eye.
As the nerve fibers pass through the lamina cribrosa sclerae they lose their medullary sheaths and are continued onward through the choroid and retina as simple axis-cylinders.
The nerve fibers forming the optic nerve exit the eye posteriorly through a hole in the sclera that is occupied by a mesh-like structure called the lamina cribrosa. It is formed by a multilayered network of collagen fibers that insert into the scleral canal wall. The nerve fibers that comprise the optic nerve run through pores formed by these collagen beams. In humans, a central retinal artery is located slightly off-center in nasal direction.

The choroid, also known as the choroidea or choroid coat, is the vascular layer of the eye, containing connective tissues, and lying between the retina and the sclera. The human choroid is thickest at the far extreme rear of the eye, while in the outlying areas it narrows to 0.1 mm. The choroid provides oxygen and nourishment to the outer layers of the retina. Along with the ciliary body and iris, the choroid forms the uveal tract.
When they reach the internal surface of the retina they radiate from their point of entrance over this surface grouped in bundles, and in many places arranged in plexuses.
Most of the fibers are centripetal, and are the direct continuations of the axis-cylinder processes of the cells of the ganglionic layer, but a few of them are centrifugal and ramify in the inner plexiform and inner nuclear layers, where they end in enlarged extremities.

In Newtonian mechanics, the centrifugal force is an inertial force that appears to act on all objects when viewed in a rotating frame of reference. It is directed away from an axis passing through the coordinate system's origin and parallel to the axis of rotation. If the axis of rotation passes through the coordinate system's origin, the centrifugal force is directed radially outwards from that axis. The concept of centrifugal force can be applied in rotating devices, such as centrifuges, centrifugal pumps, centrifugal governors, and centrifugal clutches, and in centrifugal railways, planetary orbits and banked curves, when they are analyzed in a rotating coordinate system. The term has sometimes also been used for the reactive centrifugal force that may be viewed as a reaction to a centripetal force in some circumstances.

The inner nuclear layer or layer of inner granules, of the retina, is made up of a number of closely packed cells, of which there are three varieties, viz.: bipolar cells, horizontal cells, and amacrine cells.
Patients with retinitis pigmentosa have abnormal thinning of the RNFL which correlates with the severity of the disease. [1] However the thickness of the RNFL also decreases with age and not visual acuity. [2] The sparing of this layer is important in the treatment of the disease as it is the basis for connecting retinal prostheses to the optic nerve, or implanting stem cells that could regenerate the lost photoreceptors.

Retinitis pigmentosa (RP) is a genetic disorder of the eyes that causes loss of vision. Symptoms include trouble seeing at night and decreased peripheral vision. Onset of symptoms is generally gradual. As peripheral vision worsens, people may experience "tunnel vision". Complete blindness is uncommon.
RNFL is a sensitive structure. Some process can excites its natural apoptosis. Harmful situation can make some damage on RNFL such as high intraocular pressure, high fluctuation on phase of intraocular pressure, inflammation, vascular disease and any kind of hypoxia. Gede Pardianto (2009) reported 6 cases of RNFL thickness change after the procedures of phacoemulsification. [3] Sudden intraocular fluctuation in any kind of intraocular surgeries maybe harmful to RNFL in accordance with mechanical stress on sudden compression and also ischemic effect of micro emboly as the result of the sudden decompression that may generate micro bubble that can clog micro vessels. [4]

Phacoemulsification is a modern cataract surgery in which the eye's internal lens is emulsified with an ultrasonic handpiece and aspirated from the eye. Aspirated fluids are replaced with irrigation of balanced salt solution to maintain the anterior chamber.