| Preimplantation factor | |
|---|---|
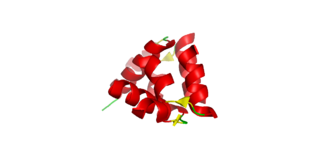
 Simulated structure of preimplantation factor | |
| Identifiers | |
| Symbol | PIF |
| Alt. names | PreImplantation factor, PIF, sPIF, PIF* |
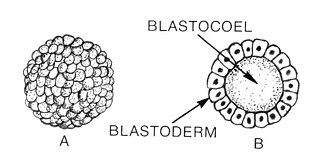
Preimplantation factor(PIF) is a peptide secreted by trophoblast cells prior to placenta formation in early embryonic development. [1] Human embryos begin to express PIF at the 4-cell stage, with expression increasing by the morula stage and continuing to do so throughout the first trimester. [2] [1] [3] Expression of preimplantation factor in the blastocyst was discovered as an early correlate of the viability of the eventual pregnancy. [1] [4] Preimplantation factor was identified in 1994 by a lymphocyte platelet-binding assay, where it was thought to be an early biomarker of pregnancy. [5] It has a simple primary structure with a short sequence of fifteen amino acids without any known quaternary structure. [6] A synthetic analogue of preimplantation factor (commonly abbreviated in studies as sPIF or PIF*) that has an identical amino acid sequence and mimics the normal biological activity of PIF has been developed and is commonly used in research studies, particularly those that aim to study potential adult therapeutics. [7] [8] [9]
Contents
- Discovery and structure
- Functions
- Trophoblast invasion and adhesion
- Maternal immune tolerance
- Viability of pregnancy
- Neurogenic and anti-apoptotic effects
- Therapeutic uses
- References
- External links
Preimplantation factor acts by paracrine signaling; that is to say trophoblast cells, which collectively form extra-embryonic tissues, secrete it onto the surface of the endometrium. PIF is known to influence many events in the implantation process, the process by which an early embryo implants into the uterine wall. A crucial event in human implantation is when trophoblast cells expressing preimplantation factor invade the uterine wall and found the placenta, an organ that connects maternal blood supply, and along with it, nutrients, to the growing fetus. This requires changes to the histology of the endometrium; a process called decidualisation. Upregulated expression of PIF increases the presence of integrins on the endometrium wall, promoting the embryo's adhesion to the uterine wall. [10] PIF is thought to modulate and facilitate the depth of the trophoblast's invasion into the uterus at physiological doses. [1]
Maternal immune system regulation is also a critical event in implantation as the early embryo is essentially a partial allograft, that is a tissue that is recognised as fully identical to that of the mother. [11] [12] Consequently, the embryo may be rejected and attacked if it is not recognised, an event that normally causes spontaneous miscarriage. [11] [12] Preimplantation factor regionally modulates the mother's immune system, decreasing the activity of peripheral maternal leukocytes, reducing inflammation and consequently also increasing the chance that the embryo will be tolerated. [13] Preimplantation factor is also an anti-apoptotic effector, maintaining the trophoblast cell integrity through the intrinsic p53 signalling pathway. [14] Moreover, preimplantation factor protects the central nervous system by downregulating pathways that promote neurone death and promoting neurogenesis. [7] [9] PIF is also known to signal against neonatal prematurity and rescues embryos from toxic uterine environments. [7] [11] [15]
Due to its multiple autoimmune and neuroprotective effects in the embryonic environment, preimplantation factor has been studied in clinical environments as a potential novel therapy for reproductive, autoimmune and neurodegenerative diseases. PIF has been successfully studied as a therapy for recurrent pregnancy loss, as it is able to rescue non-viable embryos from a hostile maternal environment. [16] It has also been shown to prevent diabetes mellitus type 1 in mice due to its ability to modulate immunological tolerance in the pancreas. [8] Finally, it reverses paralysis and neuroinflammation whilst promoting neurogenesis in adult patients with neurodegenerative diseases. [11] [17] It also may be able to decrease the severity of brain injuries by modulating the behaviour of supporting cells in the nervous system. [9]