This article needs more reliable medical references for verification or relies too heavily on primary sources .(February 2021) |

Menstruation (also known as a period, among other colloquial terms) is the regular discharge of blood and mucosal tissue from the inner lining of the uterus through the vagina. [1] The menstrual cycle is characterized by the rise and fall of hormones. [1] Menstruation is triggered by falling progesterone levels, and is a sign that pregnancy has not occurred. [1] Feminine hygiene products are used in order to maintain hygiene during menses.
Contents
- Characteristics
- Length and duration
- Menstrual fluid
- Hormonal changes
- Side effects
- Menstrual health overview
- Moods and premenstrual syndrome (PMS)
- Cramps
- Interactions with other conditions
- Sexual activity
- Fertility aspects
- Menstrual disorders
- Dysmenorrhea
- Menstrual hygiene management
- Menstrual suppression
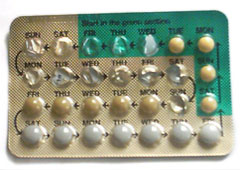
- Due to hormonal contraception
- Due to breastfeeding
- Society and culture
- Etymology and terminology
- Traditions, taboos and education
- Beliefs around synchrony
- Work
- Other mammals
- See also
- References
- Sources
- Further reading
- External links
The first period, a point in time known as menarche, usually begins during puberty, between the ages of 11 and 13. [2] However, menstruation starting as young as eight years would still be considered normal. [3] The average age of the first period is generally later in the developing world, and earlier in the developed world. [4] The typical length of time between the first day of one period and the first day of the next is 21 to 45 days in young women; in adults, the range is between 21 and 35 days with the average often cited as 28 days. [3] [4] In the largest study of menstrual app data, the mean menstrual cycle length was determined to be 29.3 days. [5] Bleeding typically lasts two to seven days. Periods stop during pregnancy and typically do not resume during the initial months of breastfeeding. [3] Lochia occurs after childbirth. [6] Menstruation, and with it the possibility of pregnancy, ceases after menopause, which usually occurs between 45 and 55 years of age. [7]
During their menstrual period, 38% of all women reported not to be able to perform all their regular daily activities. [8] Symptoms in advance of menstruation that do interfere with normal life are called premenstrual syndrome (PMS). Some 20 to 30% of women experience PMS, with 3 to 8% experiencing severe symptoms. [9] These include acne, tender breasts, bloating, feeling tired, irritability, and mood changes. [10] Other symptoms some women experience include painful periods (estimates are between 50 and 90%) and heavy bleeding during menstruation and abnormal bleeding at any time during the menstrual cycle. [3] A lack of periods, known as amenorrhea, is when periods do not occur by age 15 or have not re-occurred in ninety days. [3]