| Renal cysts and diabetes syndrome | |
|---|---|
| Other names | MODY 5 |
 | |
| MODY 5 is inherited in an autosomal dominant manner. | |
Renal cysts and diabetes syndrome (RCAD), also known as MODY 5 or HNF1B-MODY, is a form of maturity onset diabetes of the young.
| Renal cysts and diabetes syndrome | |
|---|---|
| Other names | MODY 5 |
 | |
| MODY 5 is inherited in an autosomal dominant manner. | |
Renal cysts and diabetes syndrome (RCAD), also known as MODY 5 or HNF1B-MODY, is a form of maturity onset diabetes of the young.
HNF1β-related MODY is one of the less common forms of MODY, with some distinctive clinical features, including atrophy of the pancreas and several forms of renal disease. HNF1β, also known as transcription factor 2 (TCF2), is involved in early stages of embryonic development of several organs, including the pancreas, where it contributes to differentiation of pancreatic endocrine Ngn3+ cell progenitors from non-endocrine embryonic duct cells. The gene is on chromosome 17q. [1]
The degree of insulin deficiency is variable. Diabetes can develop from infancy through middle adult life, and some family members who carry the gene remain free of diabetes into later adult life. Most of those who develop diabetes show atrophy of the entire pancreas, with mild or subclinical deficiency of exocrine as well as endocrine function.[ citation needed ]
The non-pancreatic manifestations are even more variable. Kidney and genitourinary malformation and diseases may occur, but inconsistently even within a family, and the specific conditions include a range of apparently unrelated anomalies and processes. The most common genitourinary condition is cystic kidney disease, but there are many varieties even of this. Renal effects begin with structural alterations (small kidneys, renal cysts, anomalies of the renal pelvis and calices), but a significant number develop slowly progressive chronic kidney failure associated with chronic cystic disease of the kidneys. In some cases, renal cysts may be detected in utero. Kidney disease may develop before or after hyperglycemia, and a significant number of people with MODY5 are discovered in renal clinics.
With or without kidney disease, some people with forms of HNF1β have had various minor or major anomalies of the reproductive system. Male defects have included epididymal cysts, agenesis of the vas deferens, or infertility due to abnormal spermatozoa. Affected women have been found to have vaginal agenesis, hypoplastic, or bicornuate uterus.[ citation needed ]
Liver enzyme elevations are common, but clinically significant liver disease is not. Hyperuricaemia and early onset gout have occurred.[ citation needed ]
Renal cysts and diabetes syndrome is caused by mutations in or deletions of the HNF1B gene. These can be intragenic HNF1B mutations or affect other genes as well, such as in 17q12 microdeletion syndrome.[ citation needed ]
Genetic Testing for mutations on the HNF1B gene can indicate MODY 5. The presence of familiar and individual renal problems as well as diabetes mellitus with absence of Type 1 and LADA antibodies in young individuals with a healthy lifestyle can lead to testing.[ citation needed ]
Treatment is dependent on the phenotype. Hyperglycaemia can be treated with insulin, oral medication or, according to newest data, with GLP-1 analogs. Sulfonylurea has been described as ineffective. Pancreatic exocrine insufficiency is treated with pancreatic enzymes such as Kreon. Some patients take magnesium supplementation or intravenous infusions. Patients with both kidney failure and diabetes can request a simultaneous pancreas and kidney transplant.[ citation needed ]

The endocrine system is a messenger system in an organism comprising feedback loops of hormones that are released by internal glands directly into the circulatory system and that target and regulate distant organs. In vertebrates, the hypothalamus is the neural control center for all endocrine systems.

The pancreas is an organ of the digestive system and endocrine system of vertebrates. In humans, it is located in the abdomen behind the stomach and functions as a gland. The pancreas is a mixed or heterocrine gland, i.e., it has both an endocrine and a digestive exocrine function. 99% of the pancreas is exocrine and 1% is endocrine. As an endocrine gland, it functions mostly to regulate blood sugar levels, secreting the hormones insulin, glucagon, somatostatin and pancreatic polypeptide. As a part of the digestive system, it functions as an exocrine gland secreting pancreatic juice into the duodenum through the pancreatic duct. This juice contains bicarbonate, which neutralizes acid entering the duodenum from the stomach; and digestive enzymes, which break down carbohydrates, proteins and fats in food entering the duodenum from the stomach.

A pancreas transplant is an organ transplant that involves implanting a healthy pancreas into a person who usually has diabetes.
Maturity-onset diabetes of the young (MODY) refers to any of several hereditary forms of diabetes mellitus caused by mutations in an autosomal dominant gene disrupting insulin production. Along with neonatal diabetes, MODY is a form of the conditions known as monogenic diabetes. While the more common types of diabetes involve more complex combinations of causes involving multiple genes and environmental factors, each forms of MODY are caused by changes to a single gene (monogenic). GCK-MODY and HNF1A-MODY are the most common forms.
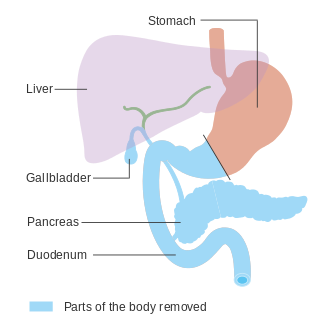
In medicine, a pancreatectomy is the surgical removal of all or part of the pancreas. Several types of pancreatectomy exist, including pancreaticoduodenectomy, distal pancreatectomy, segmental pancreatectomy, and total pancreatectomy. In total pancreatectomy, the gallbladder, distal stomach, a portion of the small intestine, associated lymph nodes and in certain cases the spleen are removed in addition to the entire pancreas. In recent years, the TP-IAT has also gained respectable traction within the medical community. These procedures are used in the management of several conditions involving the pancreas, such as benign pancreatic tumors, pancreatic cancer, and pancreatitis.

Exocrine pancreatic insufficiency (EPI) is the inability to properly digest food due to a lack or reduction of digestive enzymes made by the pancreas. EPI can occur in humans and is prevalent in many conditions such as cystic fibrosis, Shwachman–Diamond syndrome, different types of pancreatitis, multiple types of diabetes mellitus, advanced renal disease, older adults, celiac disease, IBS-D, IBD, HIV, alcohol-related liver disease, Sjogren syndrome, tobacco use, and use of somatostatin analogues.

Cystic kidney disease refers to a wide range of hereditary, developmental, and acquired conditions and with the inclusion of neoplasms with cystic changes, over 40 classifications and subtypes have been identified. Depending on the disease classification, the presentation may be at birth, or much later into adult life. Cystic disease may involve one or both kidneys and may, or may not, occur in the presence of other anomalies. A higher incidence is found in males and prevalence increases with age. Renal cysts have been reported in more than 50% of patients over the age of 50. Typically, cysts grow up to 2.88 mm annually and may cause related pain and/or hemorrhage.
Pancreatic diseases are diseases that affect the pancreas, an organ in most vertebrates and in humans and other mammals located in the abdomen. The pancreas plays a role in the digestive and endocrine system, producing enzymes which aid the digestion process and the hormone insulin, which regulates blood sugar levels. The most common pancreatic disease is pancreatitis, an inflammation of the pancreas which could come in acute or chronic form. Other pancreatic diseases include diabetes mellitus, exocrine pancreatic insufficiency, cystic fibrosis, pseudocysts, cysts, congenital malformations, tumors including pancreatic cancer, and hemosuccus pancreaticus.
Pearson syndrome is a mitochondrial disease characterized by sideroblastic anemia and exocrine pancreas dysfunction. Other clinical features are failure to thrive, pancreatic fibrosis with insulin-dependent diabetes and exocrine pancreatic deficiency, muscle and neurologic impairment, and, frequently, early death. It is usually fatal in infancy. The few patients who survive into adulthood often develop symptoms of Kearns–Sayre syndrome. It is caused by a deletion in mitochondrial DNA. Pearson syndrome is very rare: fewer than a hundred cases have been reported in medical literature worldwide.

PDX1, also known as insulin promoter factor 1, is a transcription factor in the ParaHox gene cluster. In vertebrates, Pdx1 is necessary for pancreatic development, including β-cell maturation, and duodenal differentiation. In humans this protein is encoded by the PDX1 gene, which was formerly known as IPF1. The gene was originally identified in the clawed frog Xenopus laevis and is present widely across the evolutionary diversity of bilaterian animals, although it has been lost in evolution in arthropods and nematodes. Despite the gene name being Pdx1, there is no Pdx2 gene in most animals; single-copy Pdx1 orthologs have been identified in all mammals. Coelacanth and cartilaginous fish are, so far, the only vertebrates shown to have two Pdx genes, Pdx1 and Pdx2.

HNF1 homeobox B, also known as HNF1B or transcription factor 2 (TCF2), is a human gene.

Renal–hepatic–pancreatic dysplasia is an autosomal recessive congenital disorder characterized by pancreatic fibrosis, renal dysplasia and hepatic dysgenesis. An association with NPHP3 has been described. It was characterized in 1959.
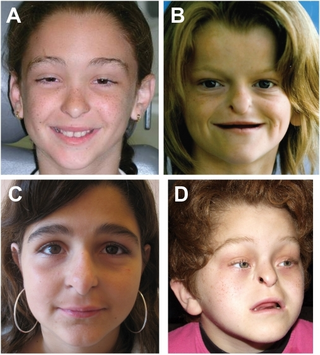
Johanson–Blizzard syndrome (JBS) is a rare, sometimes fatal autosomal recessive multisystem congenital disorder featuring abnormal development of the pancreas, nose and scalp, with intellectual disability, hearing loss and growth failure. It is sometimes described as a form of ectodermal dysplasia.
MODY 4 or PDX1-MODY is a form of maturity onset diabetes of the young.

Neurogenin-3 (NGN3) is a protein that in humans is encoded by the Neurog3 gene.
Cystic fibrosis–related diabetes (CFRD) is diabetes specifically caused by cystic fibrosis, a genetic condition. Cystic fibrosis related diabetes mellitus (CFRD) develops with age, and the median age at diagnosis is 21 years. It is an example of type 3c diabetes – diabetes that is caused by damage to the pancreas from another disease or condition.

Pancreatic progenitor cells are multipotent stem cells originating from the developing fore-gut endoderm which have the ability to differentiate into the lineage specific progenitors responsible for the developing pancreas.

17q12 microdeletion syndrome, also known as 17q12 deletion syndrome, is a rare chromosomal anomaly caused by the deletion of a small amount of material from a region in the long arm of chromosome 17. It is typified by deletion of the HNF1B gene, resulting in kidney abnormalities and renal cysts and diabetes syndrome. It also has neurocognitive effects, and has been implicated as a genetic factor for autism and schizophrenia.

Dorsal pancreatic agenesis is a congenital anomaly characterised by the absence of the duct of Santorini, tail and body of the pancreas. It is regarded as asymptomatic and the most common clinical manifestation is non-specific abdominal pain. While the cause is unclear, its mechanism is thought to be impaired dorsal buds or mutation of genes that regulate organogenesis during embryogenesis.