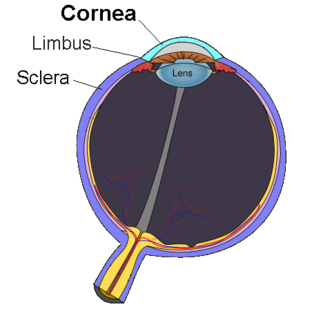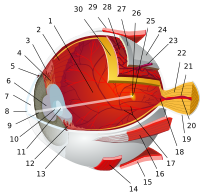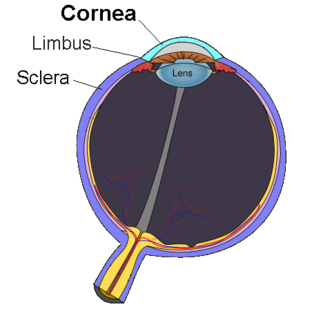
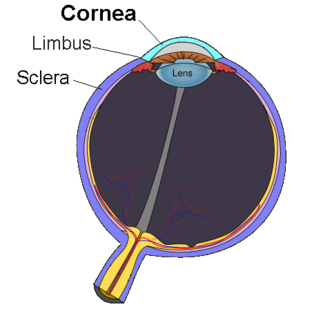
The cornea is the transparent front part of the eye that covers the iris, pupil, and anterior chamber. Along with the anterior chamber and lens, the cornea refracts light, accounting for approximately two-thirds of the eye's total optical power. In humans, the refractive power of the cornea is approximately 43 dioptres. The cornea can be reshaped by surgical procedures such as LASIK.

The corneal endothelium is a single layer of endothelial cells on the inner surface of the cornea. It faces the chamber formed between the cornea and the iris.

Corneal transplantation, also known as corneal grafting, is a surgical procedure where a damaged or diseased cornea is replaced by donated corneal tissue. When the entire cornea is replaced it is known as penetrating keratoplasty and when only part of the cornea is replaced it is known as lamellar keratoplasty. Keratoplasty simply means surgery to the cornea. The graft is taken from a recently deceased individual with no known diseases or other factors that may affect the chance of survival of the donated tissue or the health of the recipient.

Fuchs dystrophy, also referred to as Fuchs endothelial corneal dystrophy (FECD) and Fuchs endothelial dystrophy (FED), is a slowly progressing corneal dystrophy that usually affects both eyes and is slightly more common in women than in men. Although early signs of Fuchs dystrophy are sometimes seen in people in their 30s and 40s, the disease rarely affects vision until people reach their 50s and 60s.

Descemet's membrane is the basement membrane that lies between the corneal proper substance, also called stroma, and the endothelial layer of the cornea. It is composed of different kinds of collagen than the stroma. The endothelial layer is located at the posterior of the cornea. Descemet's membrane, as the basement membrane for the endothelial layer, is secreted by the single layer of squamous epithelial cells that compose the endothelial layer of the cornea.

A corneal ulcer, or ulcerative keratitis, is an inflammatory condition of the cornea involving loss of its outer layer. It is very common in dogs and is sometimes seen in cats. In veterinary medicine, the term corneal ulcer is a generic name for any condition involving the loss of the outer layer of the cornea, and as such is used to describe conditions with both inflammatory and traumatic causes.
Iridocorneal Endothelial (ICE) syndromes are a spectrum of diseases characterized by slowly progressive abnormalities of the corneal endothelium and features including corneal edema, iris distortion, and secondary angle-closure glaucoma. [1,2,4] ICE syndromes are predominantly unilateral and nonhereditary [1,2,4]. The condition occurs in predominantly middle-aged women [1,3,4].
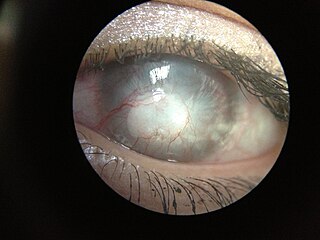
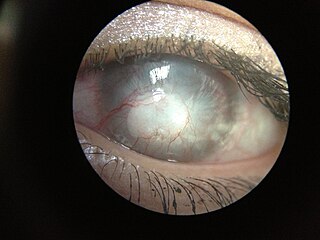
Corneal neovascularization (CNV) is the in-growth of new blood vessels from the pericorneal plexus into avascular corneal tissue as a result of oxygen deprivation. Maintaining avascularity of the corneal stroma is an important aspect of corneal pathophysiology as it is required for corneal transparency and optimal vision. A decrease in corneal transparency causes visual acuity deterioration. Corneal tissue is avascular in nature and the presence of vascularization, which can be deep or superficial, is always pathologically related.

Iridogoniodysgenesis, dominant type refers to a spectrum of diseases characterized by malformations of the irido-corneal angle of the anterior chamber of the eye. Iridogoniodysgenesis is the result of abnormal migration or terminal induction of neural crest cells. These cells lead to formation of most of the anterior segment structures of the eye.
Bullous keratopathy, also known as pseudophakic bullous keratopathy (PBK), is a pathological condition in which small vesicles, or bullae, are formed in the cornea due to endothelial dysfunction.
Interstitial keratitis (IK) is corneal scarring due to chronic inflammation of the corneal stroma. Interstitial means space between cells i.e. corneal stroma which lies between the epithelium and the endothelium. Keratitis means corneal inflammation.

Corneal keratocytes are specialized fibroblasts residing in the stroma. This corneal layer, representing about 85-90% of corneal thickness, is built up from highly regular collagenous lamellae and extracellular matrix components. Keratocytes play the major role in keeping it transparent, healing its wounds, and synthesizing its components. In the unperturbed cornea keratocytes stay dormant, coming into action after any kind of injury or inflammation. Some keratocytes underlying the site of injury, even a light one, undergo apoptosis immediately after the injury. Any glitch in the precisely orchestrated process of healing may cloud the cornea, while excessive keratocyte apoptosis may be a part of the pathological process in the degenerative corneal disorders such as keratoconus, and these considerations prompt the ongoing research into the function of these cells.

Posterior Polymorphous Corneal Dystrophy is a type of corneal dystrophy, characterised by changes in Descemet's membrane and endothelial layer. Symptoms mainly consist of decreased vision due to corneal edema. In some cases they are present from birth, other patients are asymptomatic. Histopathological analysis shows that the cells of endothelium have some characteristics of epithelial cells and have become multilayered. The disease was first described in 1916 by Koeppe as keratitis bullosa interna.

Anterior segment mesenchymal dysgenesis, or simply anterior segment dysgenesis (ASD), is a failure of the normal development of the tissues of the anterior segment of the eye. It leads to anomalies in the structure of the mature anterior segment, associated with an increased risk of glaucoma and corneal opacity.

Long-term contact lens use can lead to alterations in corneal thickness, stromal thickness, curvature, corneal sensitivity, cell density, and epithelial oxygen uptake, etc. Other changes may include the formation of epithelial vacuoles and microcysts as well as the emergence of polymegethism in the corneal endothelium. Decreased corneal sensitivity, vision loss, and photophobia have also been observed in patients who have worn contact lenses for an extended period of time. Many contact lens-induced changes in corneal structure are reversible if contact lenses are removed for an extended period of time.

Keratic precipitate (KP) is an inflammatory cellular deposit seen on corneal endothelium. Acute KPs are white and round in shape whereas old KPs are faded and irregular in shape. Mutton-fat KPs are large in shape and are greasy-white in color and are formed from macrophages and epithelioid cells. They are indicative of inflammatory disease. Mutton fat KPs are due to granulomatous iridocyclitis. Another variant called red KPs may be seen in hemorrhagic uveitis.

Herpetic simplex keratitis is a form of keratitis caused by recurrent herpes simplex virus (HSV) infection in the cornea.
Pre Descemet's endothelial keratoplasty (PDEK) is a kind of endothelial keratoplasty, where the pre descemet's layer (PDL) along with descemet's membrane (DM) and endothelium is transplanted. Conventionally in a corneal transplantation, doctors use a whole cornea or parts of the five layers of the cornea to perform correction surgeries. In May 2013, Dr Harminder Dua discovered a sixth layer between the stroma and the descemet membrane which was named after him as the Dua's layer. In the PDEK technique, doctors take the innermost two layers of the cornea, along with the Dua's layer and graft it in the patient's eye.
Tsutomu Sato was a Japanese ophthalmologist who performed an early version of the radial keratotomy and was the first professor at the Research Institute of Ophthalmology at Juntendo University School of Medicine.
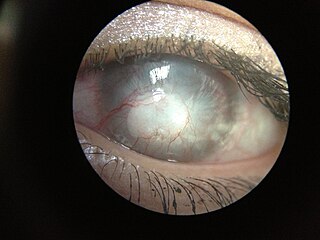
The human cornea is a transparent membrane which allows light to pass through it. The word corneal opacification literally means loss of normal transparency of cornea. The term corneal opacity is used particularly for the loss of transparency of cornea due to scarring. Transparency of the cornea is dependent on the uniform diameter and the regular spacing and arrangement of the collagen fibrils within the stroma. Alterations in the spacing of collagen fibrils in a variety of conditions including corneal edema, scars, and macular corneal dystrophy is clinically manifested as corneal opacity. The term "corneal blindness" is commonly used to describe blindness due to corneal opacity.