Cerebrospinal fluid (CSF) is a clear, colorless body fluid found within the tissue that surrounds the brain and spinal cord of all vertebrates.

Veins are blood vessels in the circulatory system of humans and most other animals that carry blood towards the heart. Most veins carry deoxygenated blood from the tissues back to the heart; exceptions are those of the pulmonary and fetal circulations which carry oxygenated blood to the heart. In the systemic circulation, arteries carry oxygenated blood away from the heart, and veins return deoxygenated blood to the heart, in the deep veins.

Coronary circulation is the circulation of blood in the arteries and veins that supply the heart muscle (myocardium). Coronary arteries supply oxygenated blood to the heart muscle. Cardiac veins then drain away the blood after it has been deoxygenated. Because the rest of the body, and most especially the brain, needs a steady supply of oxygenated blood that is free of all but the slightest interruptions, the heart is required to function continuously. Therefore its circulation is of major importance not only to its own tissues but to the entire body and even the level of consciousness of the brain from moment to moment. Interruptions of coronary circulation quickly cause heart attacks, in which the heart muscle is damaged by oxygen starvation. Such interruptions are usually caused by coronary ischemia linked to coronary artery disease, and sometimes to embolism from other causes like obstruction in blood flow through vessels.

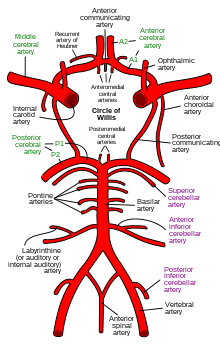
The circle of Willis is a circulatory anastomosis that supplies blood to the brain and surrounding structures in reptiles, birds and mammals, including humans. It is named after Thomas Willis (1621–1675), an English physician.

Cerebral edema is excess accumulation of fluid (edema) in the intracellular or extracellular spaces of the brain. This typically causes impaired nerve function, increased pressure within the skull, and can eventually lead to direct compression of brain tissue and blood vessels. Symptoms vary based on the location and extent of edema and generally include headaches, nausea, vomiting, seizures, drowsiness, visual disturbances, dizziness, and in severe cases, death.

Intracranial pressure (ICP) is the pressure exerted by fluids such as cerebrospinal fluid (CSF) inside the skull and on the brain tissue. ICP is measured in millimeters of mercury (mmHg) and at rest, is normally 7–15 mmHg for a supine adult. The body has various mechanisms by which it keeps the ICP stable, with CSF pressures varying by about 1 mmHg in normal adults through shifts in production and absorption of CSF.

The internal carotid artery is an artery in the neck which supplies the anterior circulation of the brain.

Intracranial hemorrhage (ICH), also known as intracranial bleed, is bleeding within the skull. Subtypes are intracerebral bleeds, subarachnoid bleeds, epidural bleeds, and subdural bleeds.

Cerebral angiography is a form of angiography which provides images of blood vessels in and around the brain, thereby allowing detection of abnormalities such as arteriovenous malformations and aneurysms. It was pioneered in 1927 by the Portuguese neurologist Egas Moniz at the University of Lisbon, who also helped develop thorotrast for use in the procedure.
Cushing reflex is a physiological nervous system response to increased intracranial pressure (ICP) that results in Cushing's triad of increased blood pressure, irregular breathing, and bradycardia. It is usually seen in the terminal stages of acute head injury and may indicate imminent brain herniation. It can also be seen after the intravenous administration of epinephrine and similar drugs. It was first described in detail by American neurosurgeon Harvey Cushing in 1901.
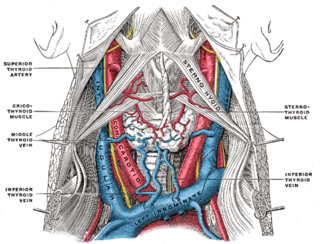
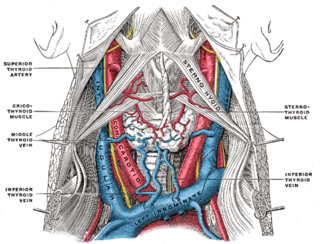
The internal jugular vein is a paired jugular vein that collects blood from the brain and the superficial parts of the face and neck. This vein runs in the carotid sheath with the common carotid artery and vagus nerve.

Intraparenchymal hemorrhage (IPH) is one form of intracerebral bleeding in which there is bleeding within brain parenchyma. The other form is intraventricular hemorrhage (IVH).
Cerebral perfusion pressure, or CPP, is the net pressure gradient causing cerebral blood flow to the brain. It must be maintained within narrow limits because too little pressure could cause brain tissue to become ischemic, and too much could raise intracranial pressure (ICP).

Cerebral infarction, also known as an ischemic stroke, is the pathologic process that results in an area of necrotic tissue in the brain. In mid to high income countries, a stroke is the main reason for disability among people and the 2nd cause of death. It is caused by disrupted blood supply (ischemia) and restricted oxygen supply (hypoxia). This is most commonly due to a thrombotic occlusion, or an embolic occlusion of major vessels which leads to a cerebral infarct. In response to ischemia, the brain degenerates by the process of liquefactive necrosis.

The leptomeningeal collateral circulation is a network of small blood vessels in the brain that connects branches of the middle, anterior and posterior cerebral arteries, with variation in its precise anatomy between individuals. During a stroke, leptomeningeal collateral vessels allow limited blood flow when other, larger blood vessels provide inadequate blood supply to a part of the brain.

Coronary perfusion pressure (CPP) refers to the pressure gradient that drives coronary blood pressure. The heart's function is to perfuse blood to the body; however, the heart's own myocardium must, itself, be supplied for its own muscle function. The heart is supplied by coronary vessels, and therefore CPP is the blood pressure within those vessels. If pressures are too low in the coronary vasculature, then the myocardium risks ischemia with subsequent myocardial infarction or cardiogenic shock.
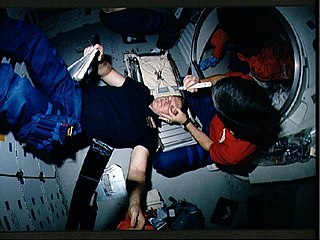
Increased intracranial pressure (ICP) is one of the major causes of secondary brain ischemia that accompanies a variety of pathological conditions, most notably traumatic brain injury (TBI), strokes, and intracranial hemorrhages. It can cause complications such as vision impairment due to intracranial pressure (VIIP), permanent neurological problems, reversible neurological problems, seizures, stroke, and death. However, aside from a few Level I trauma centers, ICP monitoring is rarely a part of the clinical management of patients with these conditions. The infrequency of ICP can be attributed to the invasive nature of the standard monitoring methods. Additional risks presented to patients can include high costs associated with an ICP sensor's implantation procedure, and the limited access to trained personnel, e.g. a neurosurgeon. Alternative, non-invasive measurement of intracranial pressure, non-invasive methods for estimating ICP have, as a result, been sought.
Cerebral autoregulation is a process in mammals that aims to maintain adequate and stable cerebral blood flow. While most systems of the body show some degree of autoregulation, the brain is very sensitive to over- and underperfusion. Cerebral autoregulation plays an important role in maintaining an appropriate blood flow to that region. Brain perfusion is essential for life, since the brain has a high metabolic demand. By means of cerebral autoregulation, the body is able to deliver sufficient blood containing oxygen and nutrients to the brain tissue for this metabolic need, and remove CO2 and other waste products.
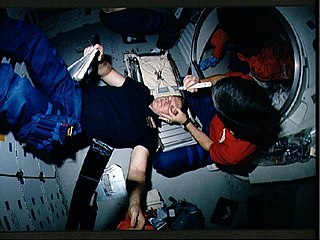
Spaceflight-associated neuro-ocular syndrome (SANS), previously called spaceflight-induced visual impairment, is hypothesized to be a result of increased intracranial pressure (ICP), although, experiments directly measuring ICP in parabolic flight have shown ICP to be in normal physiological ranges during acute weightless exposure. The study of visual changes and ICP in astronauts on long-duration flights is a relatively recent topic of interest to space medicine professionals. Although reported signs and symptoms have not appeared to be severe enough to cause blindness in the near term, long term consequences of chronically elevated intracranial pressure are unknown.

Pressure reactivity index or PRx is a tool for monitoring cerebral autoregulation in the intensive care setting for patients with severe traumatic brain injury or subarachnoid haemorrhage, in order to guide therapy to protect the brain from dangerously high or low cerebral blood flow.