Related Research Articles

A cerebral arteriovenous malformation is an abnormal connection between the arteries and veins in the brain—specifically, an arteriovenous malformation in the cerebrum.

Lemierre's syndrome is infectious thrombophlebitis of the internal jugular vein. It most often develops as a complication of a bacterial sore throat infection in young, otherwise healthy adults. The thrombophlebitis is a serious condition and may lead to further systemic complications such as bacteria in the blood or septic emboli.

Sepsis is a potentially life-threatening condition that arises when the body's response to infection causes injury to its own tissues and organs.

An intracranial aneurysm, also known as a cerebral aneurysm, is a cerebrovascular disorder characterized by a localized dilation or ballooning of a blood vessel in the brain due to a weakness in the vessel wall. These aneurysms can occur in any part of the brain but are most commonly found in the arteries of the circle of Willis. The risk of rupture varies with the size and location of the aneurysm, with those in the posterior circulation being more prone to rupture.

Cerebrovascular disease includes a variety of medical conditions that affect the blood vessels of the brain and the cerebral circulation. Arteries supplying oxygen and nutrients to the brain are often damaged or deformed in these disorders. The most common presentation of cerebrovascular disease is an ischemic stroke or mini-stroke and sometimes a hemorrhagic stroke. Hypertension is the most important contributing risk factor for stroke and cerebrovascular diseases as it can change the structure of blood vessels and result in atherosclerosis. Atherosclerosis narrows blood vessels in the brain, resulting in decreased cerebral perfusion. Other risk factors that contribute to stroke include smoking and diabetes. Narrowed cerebral arteries can lead to ischemic stroke, but continually elevated blood pressure can also cause tearing of vessels, leading to a hemorrhagic stroke.

An aneurysm is an outward bulging, likened to a bubble or balloon, caused by a localized, abnormal, weak spot on a blood vessel wall. Aneurysms may be a result of a hereditary condition or an acquired disease. Aneurysms can also be a nidus for clot formation (thrombosis) and embolization. As an aneurysm increases in size, the risk of rupture, which leads to uncontrolled bleeding, increases. Although they may occur in any blood vessel, particularly lethal examples include aneurysms of the circle of Willis in the brain, aortic aneurysms affecting the thoracic aorta, and abdominal aortic aneurysms. Aneurysms can arise in the heart itself following a heart attack, including both ventricular and atrial septal aneurysms. There are congenital atrial septal aneurysms, a rare heart defect.

Septic shock is a potentially fatal medical condition that occurs when sepsis, which is organ injury or damage in response to infection, leads to dangerously low blood pressure and abnormalities in cellular metabolism. The Third International Consensus Definitions for Sepsis and Septic Shock (Sepsis-3) defines septic shock as a subset of sepsis in which particularly profound circulatory, cellular, and metabolic abnormalities are associated with a greater risk of mortality than with sepsis alone. Patients with septic shock can be clinically identified by requiring a vasopressor to maintain a mean arterial pressure of 65 mm Hg or greater and having serum lactate level greater than 2 mmol/L (>18 mg/dL) in the absence of hypovolemia. This combination is associated with hospital mortality rates greater than 40%.

Interventional radiology (IR) is a medical specialty that performs various minimally-invasive procedures using medical imaging guidance, such as x-ray fluoroscopy, computed tomography, magnetic resonance imaging, or ultrasound. IR performs both diagnostic and therapeutic procedures through very small incisions or body orifices. Diagnostic IR procedures are those intended to help make a diagnosis or guide further medical treatment, and include image-guided biopsy of a tumor or injection of an imaging contrast agent into a hollow structure, such as a blood vessel or a duct. By contrast, therapeutic IR procedures provide direct treatment—they include catheter-based medicine delivery, medical device placement, and angioplasty of narrowed structures.

Infective endocarditis is an infection of the inner surface of the heart (endocardium), usually the valves. Signs and symptoms may include fever, small areas of bleeding into the skin, heart murmur, feeling tired, and low red blood cell count. Complications may include backward blood flow in the heart, heart failure – the heart struggling to pump a sufficient amount of blood to meet the body's needs, abnormal electrical conduction in the heart, stroke, and kidney failure.

Subarachnoid hemorrhage (SAH) is bleeding into the subarachnoid space—the area between the arachnoid membrane and the pia mater surrounding the brain. Symptoms may include a severe headache of rapid onset, vomiting, decreased level of consciousness, fever, weakness, numbness, and sometimes seizures. Neck stiffness or neck pain are also relatively common. In about a quarter of people a small bleed with resolving symptoms occurs within a month of a larger bleed.

A subdural hematoma (SDH) is a type of bleeding in which a collection of blood—usually but not always associated with a traumatic brain injury—gathers between the inner layer of the dura mater and the arachnoid mater of the meninges surrounding the brain. It usually results from tears in bridging veins that cross the subdural space.

Intracranial hemorrhage (ICH), also known as intracranial bleed, is bleeding within the skull. Subtypes are intracerebral bleeds, subarachnoid bleeds, epidural bleeds, and subdural bleeds.
A thunderclap headache is a headache that is severe and has a sudden onset. It is defined as a severe headache that takes seconds to minutes to reach maximum intensity. Although approximately 75% are attributed to "primary" headaches—headache disorder, non-specific headache, idiopathic thunderclap headache, or uncertain headache disorder—the remainder are secondary to other causes, which can include some extremely dangerous acute conditions, as well as infections and other conditions. Usually, further investigations are performed to identify the underlying cause.
Fungal keratitis is a fungal infection of the cornea, which can lead to blindness. It generally presents with a red, painful eye and blurred vision. There is also increased sensitivity to light, and excessive tears or discharge.
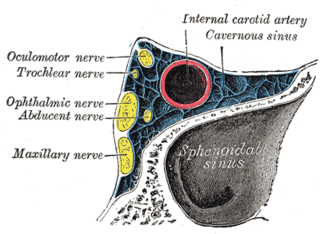
Cavernous sinus thrombosis (CST) is the formation of a blood clot within the cavernous sinus, a cavity at the base of the brain which drains deoxygenated blood from the brain back to the heart. This is a rare disorder and can be of two types–septic cavernous thrombosis and aseptic cavernous thrombosis. The most common form is septic cavernous sinus thrombosis. The cause is usually from a spreading infection in the nose, sinuses, ears, or teeth. Staphylococcus aureus and Streptococcus are often the associated bacteria.

An external ventricular drain (EVD), also known as a ventriculostomy or extraventricular drain, is a device used in neurosurgery to treat hydrocephalus and relieve elevated intracranial pressure when the normal flow of cerebrospinal fluid (CSF) inside the brain is obstructed. An EVD is a flexible plastic catheter placed by a neurosurgeon or neurointensivist and managed by intensive care unit (ICU) physicians and nurses. The purpose of external ventricular drainage is to divert fluid from the ventricles of the brain and allow for monitoring of intracranial pressure. An EVD must be placed in a center with full neurosurgical capabilities, because immediate neurosurgical intervention can be needed if a complication of EVD placement, such as bleeding, is encountered.

Meningitis is acute or chronic inflammation of the protective membranes covering the brain and spinal cord, collectively called the meninges. The most common symptoms are fever, intense headache, vomiting, and neck stiffness and occasionally photophobia.

An infected aneurysm is an aneurysm arising from bacterial infection of the arterial wall. It can be a common complication of the hematogenous spread of bacterial infection.
Anaerobic infections are caused by anaerobic bacteria. Obligately anaerobic bacteria do not grow on solid media in room air ; facultatively anaerobic bacteria can grow in the presence or absence of air. Microaerophilic bacteria do not grow at all aerobically or grow poorly, but grow better under 10% carbon dioxide or anaerobically. Anaerobic bacteria can be divided into strict anaerobes that can not grow in the presence of more than 0.5% oxygen and moderate anaerobic bacteria that are able of growing between 2 and 8% oxygen. Anaerobic bacteria usually do not possess catalase, but some can generate superoxide dismutase which protects them from oxygen.

Endovascular coiling is an endovascular treatment for intracranial aneurysms and bleeding throughout the body. The procedure reduces blood circulation to the aneurysm through the use of microsurgical detachable platinum wires, with the clinician inserting one or more into the aneurysm until it is determined that blood flow is no longer occurring within the space. It is one of two main treatments for cerebral aneurysms, the other being surgical clipping. Clipping is an alternative to stenting for bleeding.
References
- 1 2 3 4 5 Ducruet, AF; Hickman, ZL; Zacharia, BE; Narula, R; Grobelny, BT; Gorski, J; Connolly ES, Jr (January 2010). "Intracranial infectious aneurysms: a comprehensive review". Neurosurgical Review. 33 (1): 37–46. doi:10.1007/s10143-009-0233-1. PMID 19838745. S2CID 25105554.
- 1 2 Clare, CE; Barrow, DL (July 1992). "Infectious intracranial aneurysms". Neurosurgery Clinics of North America. 3 (3): 551–66. doi:10.1016/S1042-3680(18)30646-6. PMID 1633479.