Anticoagulants, commonly known as blood thinners, are chemical substances that prevent or reduce coagulation of blood, prolonging the clotting time. Some of them occur naturally in blood-eating animals such as leeches and mosquitoes, where they help keep the bite area unclotted long enough for the animal to obtain some blood. As a class of medications, anticoagulants are used in therapy for thrombotic disorders. Oral anticoagulants (OACs) are taken by many people in pill or tablet form, and various intravenous anticoagulant dosage forms are used in hospitals. Some anticoagulants are used in medical equipment, such as sample tubes, blood transfusion bags, heart–lung machines, and dialysis equipment. One of the first anticoagulants, warfarin, was initially approved as a rodenticide.

Thrombosis is the formation of a blood clot inside a blood vessel, obstructing the flow of blood through the circulatory system. When a blood vessel is injured, the body uses platelets (thrombocytes) and fibrin to form a blood clot to prevent blood loss. Even when a blood vessel is not injured, blood clots may form in the body under certain conditions. A clot, or a piece of the clot, that breaks free and begins to travel around the body is known as an embolus.
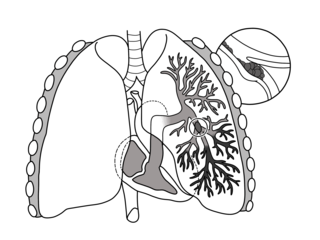
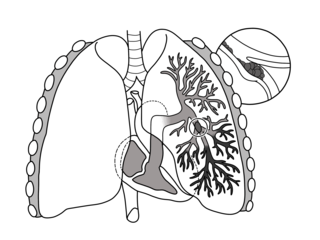
Pulmonary embolism (PE) is a blockage of an artery in the lungs by a substance that has moved from elsewhere in the body through the bloodstream (embolism). Symptoms of a PE may include shortness of breath, chest pain particularly upon breathing in, and coughing up blood. Symptoms of a blood clot in the leg may also be present, such as a red, warm, swollen, and painful leg. Signs of a PE include low blood oxygen levels, rapid breathing, rapid heart rate, and sometimes a mild fever. Severe cases can lead to passing out, abnormally low blood pressure, obstructive shock, and sudden death.

Venous thrombosis is blockage of a vein caused by a thrombus. A common form of venous thrombosis is deep vein thrombosis (DVT), when a blood clot forms in the deep veins. If a thrombus breaks off (embolizes) and flows to the lungs to lodge there, it becomes a pulmonary embolism (PE), a blood clot in the lungs. The conditions of DVT only, DVT with PE, and PE only, are all captured by the term venous thromboembolism (VTE).
Factor V Leiden is a variant of human factor V, which causes an increase in blood clotting (hypercoagulability). Due to this mutation, protein C, an anticoagulant protein that normally inhibits the pro-clotting activity of factor V, is not able to bind normally to factor V, leading to a hypercoagulable state, i.e., an increased tendency for the patient to form abnormal and potentially harmful blood clots. Factor V Leiden is the most common hereditary hypercoagulability disorder amongst ethnic Europeans. It is named after the Dutch city of Leiden, where it was first identified in 1994 by Rogier Maria Bertina under the direction of Pieter Hendrick Reitsma. Despite the increased risk of venous thromboembolisms, people with one copy of this gene have not been found to have shorter lives than the general population.

Nephrotic syndrome is a collection of symptoms due to kidney damage. This includes protein in the urine, low blood albumin levels, high blood lipids, and significant swelling. Other symptoms may include weight gain, feeling tired, and foamy urine. Complications may include blood clots, infections, and high blood pressure.

Ischemia or ischaemia is a restriction in blood supply to any tissue, muscle group, or organ of the body, causing a shortage of oxygen that is needed for cellular metabolism. Ischemia is generally caused by problems with blood vessels, with resultant damage to or dysfunction of tissue i.e. hypoxia and microvascular dysfunction. It also implies local hypoxia in a part of a body resulting from constriction. Ischemia causes not only insufficiency of oxygen, but also reduced availability of nutrients and inadequate removal of metabolic wastes. Ischemia can be partial or total blockage. The inadequate delivery of oxygenated blood to the organs must be resolved either by treating the cause of the inadequate delivery or reducing the oxygen demand of the system that needs it. For example, patients with myocardial ischemia have a decreased blood flow to the heart and are prescribed with medications that reduce chronotrophy and ionotrophy to meet the new level of blood delivery supplied by the stenosed vasculature so that it is adequate.

Deep vein thrombosis (DVT) is a type of venous thrombosis involving the formation of a blood clot in a deep vein, most commonly in the legs or pelvis. A minority of DVTs occur in the arms. Symptoms can include pain, swelling, redness, and enlarged veins in the affected area, but some DVTs have no symptoms. The most common life-threatening concern with DVT is the potential for a clot to embolize, travel as an embolus through the right side of the heart, and become lodged in a pulmonary artery that supplies blood to the lungs. This is called a pulmonary embolism (PE). DVT and PE comprise the cardiovascular disease of venous thromboembolism (VTE). About two-thirds of VTE manifests as DVT only, with one-third manifesting as PE with or without DVT. The most frequent long-term DVT complication is post-thrombotic syndrome, which can cause pain, swelling, a sensation of heaviness, itching, and in severe cases, ulcers. Recurrent VTE occurs in about 30% of those in the ten years following an initial VTE.
Low-molecular-weight heparin (LMWH) is a class of anticoagulant medications. They are used in the prevention of blood clots and treatment of venous thromboembolism and in the treatment of myocardial infarction.

Budd–Chiari syndrome is a very rare condition, affecting one in a million adults. The condition is caused by occlusion of the hepatic veins that drain the liver. The symptoms are non-specific and vary widely, but it may present with the classical triad of abdominal pain, ascites, and liver enlargement. It is usually seen in younger adults, with the median age at diagnosis between the ages of 35 and 40, and it has a similar incidence in males and females. The syndrome can be fulminant, acute, chronic, or asymptomatic. Subacute presentation is the most common form.

Thrombophilia is an abnormality of blood coagulation that increases the risk of thrombosis. Such abnormalities can be identified in 50% of people who have an episode of thrombosis that was not provoked by other causes. A significant proportion of the population has a detectable thrombophilic abnormality, but most of these develop thrombosis only in the presence of an additional risk factor.

Dalteparin is a low molecular weight heparin. It is marketed as Fragmin. Like other low molecular weight heparins, dalteparin is used for prophylaxis or treatment of deep vein thrombosis and pulmonary embolism to reduce the risk of a stroke or heart attack. Dalteparin acts by potentiating the activity of antithrombin III, inhibiting formation of both Factor Xa and thrombin. It is normally administered by self-injection.
Congenital nephrotic syndrome is a rare kidney disease which manifests in infants during the first 3 months of life, and is characterized by high levels of protein in the urine (proteinuria), low levels of protein in the blood, and swelling. This disease is primarily caused by genetic mutations which result in damage to components of the glomerular filtration barrier and allow for leakage of plasma proteins into the urinary space.
Hypercoagulability in pregnancy is the propensity of pregnant women to develop thrombosis. Pregnancy itself is a factor of hypercoagulability, as a physiologically adaptive mechanism to prevent post partum bleeding. However, when combined with an additional underlying hypercoagulable states, the risk of thrombosis or embolism may become substantial.

Cerebral venous sinus thrombosis (CVST), cerebral venous and sinus thrombosis or cerebral venous thrombosis (CVT), is the presence of a blood clot in the dural venous sinuses, the cerebral veins, or both. Symptoms may include severe headache, visual symptoms, any of the symptoms of stroke such as weakness of the face and limbs on one side of the body, and seizures, which occur in around 40% of patients.

Renal biopsy is a medical procedure in which a small piece of kidney is removed from the body for examination, usually under a microscope. Microscopic examination of the tissue can provide information needed to diagnose, monitor or treat problems of the kidney.

Arterial embolism is a sudden interruption of blood flow to an organ or body part due to an embolus adhering to the wall of an artery blocking the flow of blood, the major type of embolus being a blood clot (thromboembolism). Sometimes, pulmonary embolism is classified as arterial embolism as well, in the sense that the clot follows the pulmonary artery carrying deoxygenated blood away from the heart. However, pulmonary embolism is generally classified as a form of venous embolism, because the embolus forms in veins. Arterial embolism is the major cause of infarction.
Blood clots are a relatively common occurrence in the general population and are seen in approximately 1-2% of the population by age 60. Typically, blood clots develop in the deep veins of the lower extremities, deep vein thrombosis (DVT) or as a blood clot in the lung, pulmonary embolism. A very small number of people who develop blood clots have a more serious and often life-threatening condition, known as thrombotic storm (TS). TS is characterized by the development of more than one blood clot in a short period of time. These clots often occur in multiple and sometimes unusual locations in the body and are often difficult to treat. TS may be associated with an existing condition or situation that predisposes a person to blood clots, such as injury, infection, or pregnancy. In many cases, a risk assessment will identify interventions that will prevent the formation of blood clots.
Prothrombin G20210A is a genetic condition that increases the risk of blood clots including from deep vein thrombosis, and of pulmonary embolism. One copy of the mutation increases the risk of a blood clot from 1 in 1,000 per year to 2.5 in 1,000. Two copies increases the risk to up to 20 in 1,000 per year. Most people never develop a blood clot in their lifetimes.

Thrombosis prevention or thromboprophylaxis is medical treatment to prevent the development of thrombosis in those considered at risk for developing thrombosis. Some people are at a higher risk for the formation of blood clots than others, such as those with cancer undergoing a surgical procedure. Prevention measures or interventions are usually begun after surgery as the associated immobility will increase a person's risk.