| Hemophilia C | |
|---|---|
| Other names | Plasma thromboplastin antecedent (PTA) deficiency, Rosenthal syndrome |
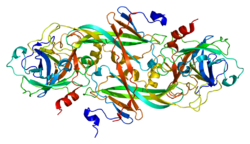 | |
| Haemophilia C caused by deficiency in Factor XI [1] | |
| Specialty | Haematology |
| Symptoms | Oral bleeding [2] |
| Causes | Deficiency of coagulation factor XI [1] |
| Diagnostic method | Prothrombin time [1] |
| Prevention | Physical activity precautions [1] |
| Treatment | tranexamic acid [3] |
Haemophilia C (also known as plasma thromboplastin antecedent (PTA) deficiency or Rosenthal syndrome) is a mild form of haemophilia affecting both sexes, due to factor XI deficiency. [4] It predominantly occurs in Ashkenazi Jews. It is the fourth most common inborn bleeding disorder after von Willebrand's disease and haemophilia A and B. In the United States, it is thought to affect 1 in 100,000 of the adult population, making it 10% as common as haemophilia A. [1] [5]


