Beta blockers, also spelled β-blockers, are a class of medications that are predominantly used to manage abnormal heart rhythms (arrhythmia), and to protect the heart from a second heart attack after a first heart attack. They are also widely used to treat high blood pressure, although they are no longer the first choice for initial treatment of most patients.

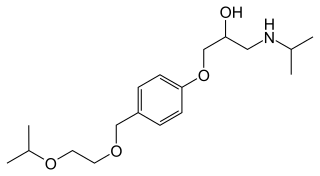
Propranolol, sold under the brand name Inderal among others, is a medication of the beta blocker class. It is used to treat high blood pressure, a number of types of irregular heart rate, thyrotoxicosis, capillary hemangiomas, performance anxiety, and essential tremors, as well to prevent migraine headaches, and to prevent further heart problems in those with angina or previous heart attacks. It can be taken orally or by intravenous injection. The formulation that is taken orally comes in short-acting and long-acting versions. Propranolol appears in the blood after 30 minutes and has a maximum effect between 60 and 90 minutes when taken orally.
Antihypertensives are a class of drugs that are used to treat hypertension. Antihypertensive therapy seeks to prevent the complications of high blood pressure, such as stroke, heart failure, kidney failure and myocardial infarction. Evidence suggests that reduction of the blood pressure by 5 mmHg can decrease the risk of stroke by 34% and of ischaemic heart disease by 21%, and can reduce the likelihood of dementia, heart failure, and mortality from cardiovascular disease. There are many classes of antihypertensives, which lower blood pressure by different means. Among the most important and most widely used medications are thiazide diuretics, calcium channel blockers, ACE inhibitors, angiotensin II receptor antagonists (ARBs), and beta blockers.
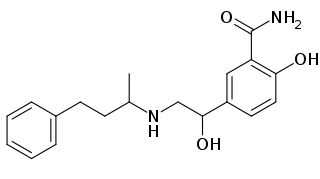
Atenolol is a beta blocker medication primarily used to treat high blood pressure and heart-associated chest pain. Although used to treat high blood pressure, it does not seem to improve mortality in those with the condition. Other uses include the prevention of migraines and treatment of certain irregular heart beats. It is taken orally or by intravenous injection. It can also be used with other blood pressure medications.

Metoprolol, sold under the brand name Lopressor among others, is a medication used to treat high blood pressure, angina, and a number of conditions involving an abnormally fast heart rate. It is also used to prevent further heart problems after myocardial infarction and to prevent headaches in those with migraines. It is a selective β1 receptor blocker medication. It is taken by mouth or is given intravenously.

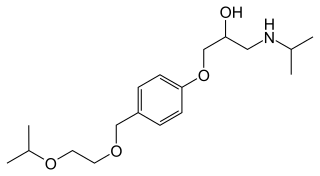
Nadolol, sold under the brand name Corgard among others, is a medication used to treat high blood pressure, heart pain, atrial fibrillation, and some inherited arrhythmic syndromes. It has also been used to prevent migraine headaches and complications of cirrhosis. It is taken orally.

Doxazosin, sold under the brand names Cardura among others, is a medication used to treat symptoms of benign prostatic hyperplasia, hypertension, and posttraumatic stress disorder (PTSD). For high blood pressure, it is a less preferred option. It is taken by mouth.

Prazosin, sold under the brand name Minipress among others, is a medication used to treat high blood pressure, symptoms of an enlarged prostate, and nightmares related to post-traumatic stress disorder (PTSD). It is an α1 blocker. It is a less preferred treatment of high blood pressure. Other uses may include heart failure and Raynaud syndrome. It is taken by mouth.

Isoprenaline, also known as isoproterenol and sold under the brand name Isuprel among others, is a sympathomimetic medication which is used in the treatment of acute bradycardia, heart block, and rarely for asthma, among other indications. It is used by injection into a vein, muscle, fat, or the heart, by inhalation, and in the past under the tongue or into the rectum.
Alpha-1 blockers constitute a variety of drugs that block the effect of catecholamines on alpha-1-adrenergic receptors. They are mainly used to treat benign prostatic hyperplasia (BPH), hypertension and post-traumatic stress disorder. Alpha-1 adrenergic receptors are present in vascular smooth muscle, the central nervous system, and other tissues. When alpha blockers bind to these receptors in vascular smooth muscle, they cause vasodilation.
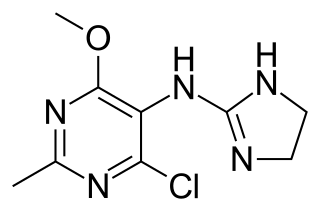
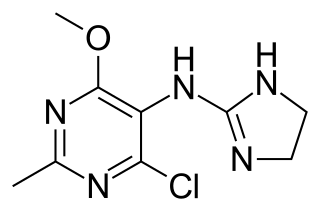
Moxonidine (INN) is a new-generation alpha-2/imidazoline receptor agonist antihypertensive drug licensed for the treatment of mild to moderate essential hypertension. It may have a role when thiazides, beta-blockers, ACE inhibitors, and calcium channel blockers are not appropriate or have failed to control blood pressure. In addition, it demonstrates favourable effects on parameters of the insulin resistance syndrome, apparently independent of blood pressure reduction. It is also a growth hormone releaser. It is manufactured by Solvay Pharmaceuticals under the brand name Physiotens and Moxon.
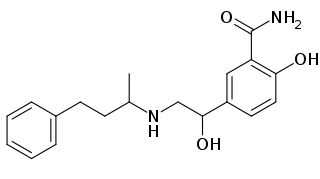
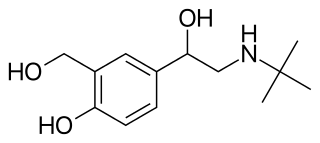
Labetalol is a medication used to treat high blood pressure and in long term management of angina. This includes essential hypertension, hypertensive emergencies, and hypertension of pregnancy. In essential hypertension it is generally less preferred than a number of other blood pressure medications. It can be given by mouth or by injection into a vein.
Bisoprolol, sold under the brand name Zebeta among others, is a beta blocker which is selective for the beta-1 receptor and used for cardiovascular diseases, including tachyarrhythmias, high blood pressure, angina, and heart failure. It is taken by mouth.

Penbutolol is a medication in the class of beta blockers, used in the treatment of high blood pressure. Penbutolol is able to bind to both beta-1 adrenergic receptors and beta-2 adrenergic receptors, thus making it a non-selective β blocker. Penbutolol is a sympathomimetic drug with properties allowing it to act as a partial agonist at β adrenergic receptors.

The beta-1 adrenergic receptor, also known as ADRB1, can refer to either the protein-encoding gene or one of the four adrenergic receptors. It is a G-protein coupled receptor associated with the Gs heterotrimeric G-protein that is expressed predominantly in cardiac tissue. In addition to cardiac tissue, beta-1 adrenergic receptors are also expressed in the cerebral cortex.

Nebivolol is a beta blocker used to treat high blood pressure and heart failure. As with other β-blockers, it is generally a less preferred treatment for high blood pressure. It may be used by itself or with other blood pressure medication. It is taken by mouth.

An adrenergic antagonist is a drug that inhibits the function of adrenergic receptors. There are five adrenergic receptors, which are divided into two groups. The first group of receptors are the beta (β) adrenergic receptors. There are β1, β2, and β3 receptors. The second group contains the alpha (α) adrenoreceptors. There are only α1 and α2 receptors. Adrenergic receptors are located near the heart, kidneys, lungs, and gastrointestinal tract. There are also α-adreno receptors that are located on vascular smooth muscle.

Alpha-blockers, also known as α-blockers or α-adrenoreceptor antagonists, are a class of pharmacological agents that act as antagonists on α-adrenergic receptors (α-adrenoceptors).
Beta adrenergic agonists or beta agonists are medications that relax muscles of the airways, causing widening of the airways and resulting in easier breathing. They are a class of sympathomimetic agents, each acting upon the beta adrenoceptors. In general, pure beta-adrenergic agonists have the opposite function of beta blockers: beta-adrenoreceptor agonist ligands mimic the actions of both epinephrine- and norepinephrine- signaling, in the heart and lungs, and in smooth muscle tissue; epinephrine expresses the higher affinity. The activation of β1, β2 and β3 activates the enzyme, adenylate cyclase. This, in turn, leads to the activation of the secondary messenger cyclic adenosine monophosphate (cAMP); cAMP then activates protein kinase A (PKA) which phosphorylates target proteins, ultimately inducing smooth muscle relaxation and contraction of the cardiac tissue.

β adrenergic receptor antagonists were initially developed in the 1960s, for the treatment of angina pectoris but are now also used for hypertension, congestive heart failure and certain arrhythmias. In the 1950s, dichloroisoproterenol (DCI) was discovered to be a β-antagonist that blocked the effects of sympathomimetic amines on bronchodilation, uterine relaxation and heart stimulation. Although DCI had no clinical utility, a change in the compound did provide a clinical candidate, pronethalol, which was introduced in 1962.