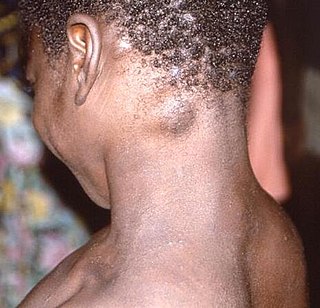
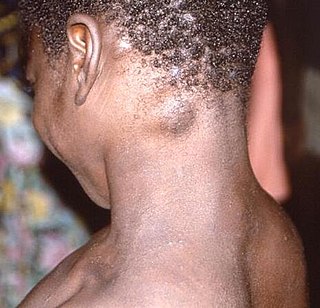
Mpox is an infectious viral disease that can occur in humans and other animals. Symptoms include a rash that forms blisters and then crusts over, fever, and swollen lymph nodes. The illness is usually mild, and most of infected individuals recover within a few weeks without treatment. The time from exposure to the onset of symptoms ranges from five to twenty-one days, and symptoms typically last from two to four weeks. However, cases may be severe, especially in children, pregnant women, or people with suppressed immune systems.

The monkeypox virus is a species of double-stranded DNA virus that causes mpox disease in humans and other mammals. It is a zoonotic virus belonging to the Orthopoxvirus genus, making it closely related to the variola, cowpox, and vaccinia viruses. MPV is oval, with a lipoprotein outer membrane. The genome is approximately 190 kb. Smallpox and monkeypox viruses are both orthopoxviruses, and the smallpox vaccine is effective against mpox if given within 3–5 years before the disease is contracted. Symptoms of mpox in humans include a rash that forms blisters and then crusts over, fever, and swollen lymph nodes. The virus is transmissible between animals and humans by direct contact to the lesions or bodily fluids. The virus was given the name monkeypox virus after being isolated from monkeys, but most of the carriers of this virus are smaller mammals.

A public health emergency of international concern is a formal declaration by the World Health Organization (WHO) of "an extraordinary event which is determined to constitute a public health risk to other States through the international spread of disease and to potentially require a coordinated international response", formulated when a situation arises that is "serious, sudden, unusual, or unexpected", which "carries implications for public health beyond the affected state's national border" and "may require immediate international action". Under the 2005 International Health Regulations (IHR), states have a legal duty to respond promptly to a PHEIC. The declaration is publicized by an IHR Emergency Committee (EC) of international experts, which was developed following the 2002–2004 SARS outbreak.

On 11 May 2017, the Democratic Republic of the Congo (DRC) was identified by the World Health Organization (WHO) as having one Ebola-related death.

The 2018 Équateur province Ebola outbreak occurred in the north-west of the Democratic Republic of the Congo (DRC) from May to July 2018. It was contained entirely within Équateur province, and was the first time that vaccination with the rVSV-ZEBOV Ebola vaccine had been attempted in the early stages of an Ebola outbreak, with a total of 3,481 people vaccinated. It was the ninth recorded Ebola outbreak in the DRC.

The Kivu Ebola epidemic was an outbreak of Ebola virus disease (EVD) mainly in eastern Democratic Republic of the Congo (DRC), and in other parts of Central Africa, from 2018 to 2020. Between 1 August 2018 and 25 June 2020 it resulted in 3,470 reported cases. The Kivu outbreak also affected Ituri Province, whose first case was confirmed on 13 August 2018. In November 2018, the outbreak became the biggest Ebola outbreak in the DRC's history, and had become the second-largest Ebola outbreak in recorded history worldwide, behind only the 2013–2016 Western Africa epidemic. In June 2019, the virus reached Uganda, having infected a 5-year-old Congolese boy who entered Uganda with his family, but was contained.

In May 2022, the World Health Organization (WHO) made an emergency announcement of the existence of a multi-country outbreak of mpox, a viral disease then commonly known as "monkeypox". The initial cluster of cases was found in the United Kingdom, where the first case was detected in London on 6 May 2022 in a patient with a recent travel history from Nigeria where the disease has been endemic. On 16 May, the UK Health Security Agency (UKHSA) confirmed four new cases with no link to travel to a country where mpox is endemic. Subsequently, cases have been reported from many countries and regions. The outbreak marked the first time mpox had spread widely outside Central and West Africa. The disease had been circulating and evolving in human hosts over several years before the outbreak and was caused by the clade IIb variant of the virus.

The 2022–2023 mpox outbreak in the United Kingdom is part of the larger outbreak of human mpox caused by the West African clade (type) of the monkeypox virus. The United Kingdom was the first country, outside of the endemic African areas, to experience an outbreak. As of 22 July 2022, there were 2,208 confirmed cases in the United Kingdom, with 2,115 in England, 54 in Scotland, 24 in Wales, and 15 in Northern Ireland.

The 2022–2023 mpox outbreak in the United States is part of the larger outbreak of human mpox caused by the West African clade of the monkeypox virus. The United States was the fourth country outside of the African countries with endemic mpox, to experience an outbreak in 2022. The first case was documented in Boston, Massachusetts, on May 17, 2022. As of August 22, mpox has spread to all 50 states in the United States, as well as Washington, D.C., and Puerto Rico. The United States has the highest number of mpox cases in the world. California has the highest number of mpox cases in the United States.

The 2022–2023 mpox outbreak in Canada is a part of the outbreak of human mpox caused by the West African clade of the monkeypox virus. The outbreak started in Canada on May 19, 2022, with the country since then becoming one of the most affected in the Americas.
The 2022 – 2023 mpox outbreak in France is part of the larger outbreak of human mpox caused by the West African clade of the monkeypox virus. France had its first case on 20 May 2022.
The 2022–2023 mpox outbreak in Belgium is part of the larger outbreak of human mpox caused by the West African clade of the monkeypox virus. Belgium was the fifth country, outside of the African countries with endemic mpox, to experience an outbreak in 2022. The first case was documented in Antwerp, Belgium, on 19 May 2022. As of 10 August, Belgium has 546 cases and 1 suspected case.
The 2022–2023 mpox outbreak in Israel is a part of the ongoing outbreak of human mpox caused by the West African clade of the monkeypox virus. The outbreak was first reported in Israel on 20 May 2022 when the Health Ministry announced a suspected case which was confirmed on 21 May 2022. One month later, on 21 June, the first locally transmitted case was reported.
The 2022–2023 mpox outbreak in Switzerland is a part of the outbreak of human mpox caused by the West African clade of the monkeypox virus. The outbreak started in Switzerland on 19 May 2022, with the country since then becoming one of the most affected in Europe.

The 2022–2023 mpox outbreak in Brazil is a part of the ongoing outbreak of human mpox caused by the West African clade of the monkeypox virus. The outbreak was first reported in Brazil on 9 June 2022 when a man in São Paulo was registered as the country's index case.
Mpox is endemic in western and central Africa, with the overwhelming majority of cases occurring in the Democratic Republic of the Congo (DRC), where the more virulent clade Ib has seen a rapid rise in infections since September 2023.

The 2022 mpox outbreak in Asia is a part of the ongoing outbreak of human mpox caused by the West African clade of the monkeypox virus. The outbreak was reported in Asia on 20 May 2022 when Israel reported a suspected case of mpox, which was confirmed on 21 May. As of 10 August 2022, seven West Asian, three Southeast Asian, three East Asian and one South Asian country, along with Russia, have reported confirmed cases.
The 2022–2023 mpox outbreak in Taiwan is a part of the larger outbreak of human mpox caused by the West African clade of the monkeypox virus. According to the Centers for Disease Control, Taiwan's first mpox case was reported on 24 June 2022.
The 2022–2023 mpox outbreak in South America is a part of the outbreak of human mpox caused by the West African clade of the monkeypox virus. The outbreak reached South America on 27 May 2022 when Argentina reported their first case of mpox. As of 14 August 2022, 8 South American countries and territories have confirmed cases.
This article documents the chronology and epidemiology of the ongoing 2023 mpox epidemic, an outbreak of clade Ib of mpox.