Related Research Articles

Coccidioidomycosis, commonly known as cocci, Valley fever, as well as California fever, desert rheumatism, or San Joaquin Valley fever, is a mammalian fungal disease caused by Coccidioides immitis or Coccidioides posadasii. Coccidioidomycosis is endemic in certain parts of the United States in Arizona, California, Nevada, New Mexico, Texas, Utah, and northern Mexico.

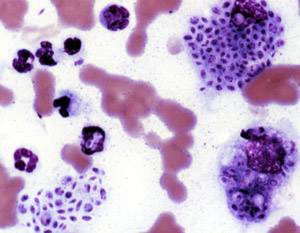
Cryptococcosis is a potentially fatal fungal infection of mainly the lungs, presenting as a pneumonia, and brain, where it appears as a meningitis. Cough, difficulty breathing, chest pain and fever are seen when the lungs are infected. When the brain is infected, symptoms include headache, fever, neck pain, nausea and vomiting, light sensitivity and confusion or changes in behavior. It can also affect other parts of the body including skin, where it may appear as several fluid-filled nodules with dead tissue.

Coccidioides immitis is a pathogenic fungus that resides in the soil in certain parts of the southwestern United States, northern Mexico, and a few other areas in the Western Hemisphere.

Blastomycosis or blasto is a fungal infection caused by inhaling spores of a Blastomyces fungus. Only about half of people with the disease have symptoms, which can include fever, cough, night sweats, muscle pains, weight loss, chest pain, and feeling tired. Symptoms usually develop between three weeks and three months after breathing in the spores. Most blastomycosis infections affect the lungs. In 25 to 40% of cases, the infection also spreads to other parts of the body, such as the skin, bones or central nervous system. Although blastomycosis is especially dangerous for those with weak immune systems, most people diagnosed with blastomycosis have healthy immune systems.

Fungal infection, also known as mycosis, is a disease caused by fungi. Different types are traditionally divided according to the part of the body affected; superficial, subcutaneous, and systemic. Superficial fungal infections include common tinea of the skin, such as tinea of the body, groin, hands, feet and beard, and yeast infections such as pityriasis versicolor. Subcutaneous types include eumycetoma and chromoblastomycosis, which generally affect tissues in and beneath the skin. Systemic fungal infections are more serious and include cryptococcosis, histoplasmosis, pneumocystis pneumonia, aspergillosis and mucormycosis. Signs and symptoms range widely. There is usually a rash with superficial infection. Fungal infection within the skin or under the skin may present with a lump and skin changes. Pneumonia-like symptoms or meningitis may occur with a deeper or systemic infection.

Pneumocystosis is a fungal infection that most often presents as Pneumocystis pneumonia in people with HIV/AIDS or poor immunity. It usually causes cough, difficulty breathing and fever, and can lead to respiratory failure. Involvement outside the lungs is rare but, can occur as a disseminated type affecting lymph nodes, spleen, liver, bone marrow, eyes, kidneys, thyroid, gastrointestinal tract or other organs. If occurring in the skin, it usually presents as nodular growths in the ear canals or underarms.
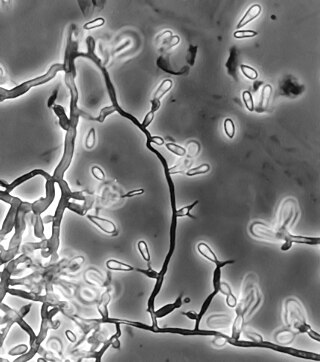
Sporotrichosis, also known as rose handler's disease, is a fungal infection that affects skin, lungs, bone and joint, and can be widespread. It presents with firm painless nodules that later ulcerate. It can be localized or widespread. The disease progresses over a week to several months after the initial exposure to the fungus. Serious complications can also develop in people who have a weakened immune system.
Talaromycosis is a fungal infection that presents with painless skin lesions of face and neck, fever, anaemia, large lymph glands and liver.

Paracoccidioidomycosis (PCM), also known as South American blastomycosis, is a fungal infection that can occur as a mouth and skin type, lymphangitic type, multi-organ involvement type, or mixed type. If there are mouth ulcers or skin lesions, the disease is likely to be widespread. There may be no symptoms, or it may present with fever, sepsis, weight loss, large glands, or a large liver and spleen.

Basidiobolomycosis is a fungal disease caused by Basidiobolus ranarum. It may appear as one or more painless firm nodules in the skin which becomes purplish with an edge that appears to be slowly growing outwards. A serious but less common type affects the stomach and intestine, which usually presents with tummy ache, fever and a lump.

Histoplasma capsulatum is a species of dimorphic fungus. Its sexual form is called Ajellomyces capsulatus. It can cause pulmonary and disseminated histoplasmosis.

Blastomyces dermatitidis is a dimorphic fungus that causes blastomycosis, an invasive and often serious fungal infection found occasionally in humans and other animals. It lives in soil and wet, decaying wood, often in an area close to a waterway such as a lake, river or stream. Indoor growth may also occur, for example, in accumulated debris in damp sheds or shacks. The fungus is endemic to parts of eastern North America, particularly boreal northern Ontario, southeastern Manitoba, Quebec south of the St. Lawrence River, parts of the U.S. Appalachian mountains and interconnected eastern mountain chains, the west bank of Lake Michigan, the state of Wisconsin, and the entire Mississippi Valley including the valleys of some major tributaries such as the Ohio River. In addition, it occurs rarely in Africa both north and south of the Sahara Desert, as well as in the Arabian Peninsula and the Indian subcontinent. Though it has never been directly observed growing in nature, it is thought to grow there as a cottony white mold, similar to the growth seen in artificial culture at 25 °C (77 °F). In an infected human or animal, however, it converts in growth form and becomes a large-celled budding yeast. Blastomycosis is generally readily treatable with systemic antifungal drugs once it is correctly diagnosed; however, delayed diagnosis is very common except in highly endemic areas.

Dimorphic fungi are fungi that can exist in the form of both mold and yeast. This is usually brought about by change in temperature and the fungi are also described as thermally dimorphic fungi. An example is Talaromyces marneffei, a human pathogen that grows as a mold at room temperature, and as a yeast at human body temperature.
Pathogenic fungi are fungi that cause disease in humans or other organisms. Approximately 300 fungi are known to be pathogenic to humans. Markedly more fungi are known to be pathogenic to plant life than those of the animal kingdom. The study of fungi pathogenic to humans is called "medical mycology". Although fungi are eukaryotic, many pathogenic fungi are microorganisms. The study of fungi and other organisms pathogenic to plants is called plant pathology.
Ochroconis gallopava, also called Dactylaria gallopava or Dactylaria constricta var. gallopava, is a member of genus Dactylaria. Ochroconis gallopava is a thermotolerant, darkly pigmented fungus that causes various infections in fowls, turkeys, poults, and immunocompromised humans first reported in 1986. Since then, the fungus has been increasingly reported as an agent of human disease especially in recipients of solid organ transplants. Ochroconis gallopava infection has a long onset and can involve a variety of body sites. Treatment of infection often involves a combination of antifungal drug therapy and surgical excision.
Emmonsia parva is a filamentous, saprotrophic fungus and one of three species within the genus Emmonsia. The fungus is most known for its causal association with the lung disease, adiaspiromycosis which occurs most commonly in small mammals but is also seen in humans. The disease was first described from rodents in Arizona, and the first human case was reported in France in 1964. Since then, the disease has been reported from Honduras, Brazil, the Czech Republic, Russia, the United States of America and Guatemala. Infections in general are quite rare, especially in humans.
Histoplasma duboisii is a saprotrophic fungus responsible for the invasive infection known as African histoplasmosis. This species is a close relative of Histoplasma capsulatum, the agent of classical histoplasmosis, and the two occur in similar habitats. Histoplasma duboisii is restricted to continental Africa and Madagascar, although scattered reports have arisen from other places usually in individuals with an African travel history. Like, H. capsulatum, H. duboisii is dimorphic – growing as a filamentous fungus at ambient temperature and a yeast at body temperature. It differs morphologically from H. capsulatum by the typical production of a large-celled yeast form. Both agents cause similar forms of disease, although H. duboisii predominantly causes cutaneous and subcutaneous disease in humans and non-human primates. The agent responds to many antifungal drug therapies used to treat serious fungal diseases.
Edouard Drouhet was a physician, biologist, and medical mycologist who played a key role in understanding how anti-fungal agents such as ketoconazole and amphotericin-B can be used as therapeutic treatments in humans with superficial or deep-seated mycoses.

Chester Wilson Emmons was an American scientist, who researched fungi that cause diseases. He was the first mycologist at the National Institutes of Health (NIH), where for 31 years he served as head of its Medical Mycology Section.
Sporothrix brasiliensis is a fungus that is commonly found in soil. It is an emerging fungal pathogen that is causing disease in humans and cats mainly in Brazil and other countries in South America.
References
- 1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 Schwartz, Ilan S.; Govender, Nelesh P.; Sigler, Lynne; Jiang, Yanping; Maphanga, Tsidiso G.; Toplis, Barbra; Botha, Alfred; Dukik, Karolina; Hoving, J. Claire; Muñoz, Jose F.; Hoog, Sybren de; Cuomo, Christina A.; Colebunders, Robert; Kenyon, Chris (19 September 2019). "Emergomyces: The global rise of new dimorphic fungal pathogens". PLOS Pathogens. 15 (9): e1007977. doi:10.1371/journal.ppat.1007977. ISSN 1553-7374. PMC 6752945 . PMID 31536607.
- 1 2 3 4 "ICD-11 - ICD-11 for Mortality and Morbidity Statistics". icd.who.int. Retrieved 28 May 2021.
- 1 2 3 4 5 6 7 8 9 10 11 12 Samaddar, Arghadip; Sharma, Anuradha (2021). "Emergomycosis, an Emerging Systemic Mycosis in Immunocompromised Patients: Current Trends and Future Prospects". Frontiers in Medicine. 8: 670731. doi: 10.3389/fmed.2021.670731 . ISSN 2296-858X. PMC 8104006 . PMID 33968970.
- 1 2 3 4 Kutzner, Heinz; Kempf, Werner; Feit, Josef; Sangueza, Omar (2021). "2. Fungal infections". Atlas of Clinical Dermatopathology: Infectious and Parasitic Dermatoses. Hoboken: Wiley Blackwell. p. 102. ISBN 978-1-119-64706-5.
- 1 2 3 4 5 6 Schwartz, Ilan S.; Govender, Nelesh P.; Corcoran, Craig; Dlamini, Sipho; Prozesky, Hans; Burton, Rosie; Mendelson, Marc; Taljaard, Jantjie; Lehloenya, Rannakoe; Calligaro, Greg; Colebunders, Robert; Kenyon, Chris (15 September 2015). "Clinical Characteristics, Diagnosis, Management, and Outcomes of Disseminated Emmonsiosis: A Retrospective Case Series". Clinical Infectious Diseases. 61 (6): 1004–1012. doi: 10.1093/cid/civ439 . ISSN 1537-6591. PMID 26060283.
- 1 2 3 4 Calonje, J. Eduardo; Grayson, Wayne (2020). "18. Infectious diseases of the skin". In Calonje, J. Eduardo; Brenn, Thomas; Lazar, Alexander J.; Billings, Steven D. (eds.). McKee's Pathology of the Skin, 2 Volume Set (5th ed.). Elsevier. pp. 959–960. ISBN 978-0-7020-6983-3.
- ↑ Govender, Nelesh P.; Grayson, Wayne (2019). "Emergomycosis (Emergomyces africanus) in Advanced HIV Disease". Dermatopathology. 6 (2): 63–69. doi:10.1159/000495405. ISSN 2296-3529. PMC 6827448 . PMID 31700845.
- ↑ Jiang, Yanping; Dukik, Karolina; Muñoz, Jose F.; Sigler, Lynne; Schwartz, Ilan S.; Govender, Nelesh P.; Kenyon, Chris; Feng, Peiying; van den Ende, Bert Gerrits; Stielow, J. Benjamin; Stchigel, Alberto M.; Lu, Hongguang; de Hoog, Sybren (1 May 2018). "Phylogeny, ecology and taxonomy of systemic pathogens and their relatives in Ajellomycetaceae (Onygenales): Blastomyces, Emergomyces, Emmonsia, Emmonsiellopsis". Fungal Diversity. 90 (1): 245–291. doi:10.1007/s13225-018-0403-y. hdl: 10067/1520590151162165141 . ISSN 1878-9129. S2CID 46987097.
- ↑ Henry, Ronnie Etymologia: Emmonsia. Emerging Infectious Diseases. 2017;23(2):348. doi:10.3201/eid2302.et2302.