Keratoconus (KC) is a disorder of the eye that results in progressive thinning of the cornea. This may result in blurry vision, double vision, nearsightedness, irregular astigmatism, and light sensitivity leading to poor quality-of-life. Usually both eyes are affected. In more severe cases a scarring or a circle may be seen within the cornea.
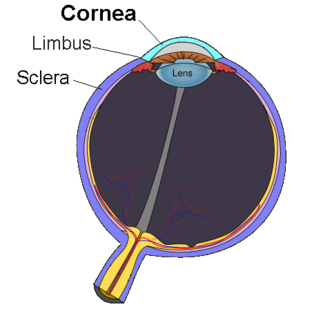
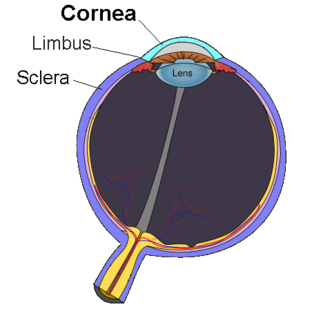
The cornea is the transparent front part of the eye that covers the iris, pupil, and anterior chamber. The cornea, with the anterior chamber and lens, refracts light, with the cornea accounting for approximately two-thirds of the eye's total optical power. In humans, the refractive power of the cornea is approximately 43 dioptres. The cornea can be reshaped by surgical procedures such as LASIK.

Eye surgery, also known as ocular surgery, is surgery performed on the eye or its adnexa, typically by an ophthalmologist. The eye is a very fragile organ, and requires extreme care before, during, and after a surgical procedure to minimise or prevent further damage. An expert eye surgeon is responsible for selecting the appropriate surgical procedure for the patient, and for taking the necessary safety precautions. Mentions of eye surgery can be found in several ancient texts dating back as early as 1800 BC, with cataract treatment starting in the fifth century BC. Today it continues to be a widely practiced type of surgery, with various techniques having been developed for treating eye problems.

The corneal endothelium is a single layer of endothelial cells on the inner surface of the cornea. It faces the chamber formed between the cornea and the iris.

A red eye is an eye that appears red due to illness or injury. It is usually injection and prominence of the superficial blood vessels of the conjunctiva, which may be caused by disorders of these or adjacent structures. Conjunctivitis and subconjunctival hemorrhage are two of the less serious but more common causes.

Corneal transplantation, also known as corneal grafting, is a surgical procedure where a damaged or diseased cornea is replaced by donated corneal tissue. When the entire cornea is replaced it is known as penetrating keratoplasty and when only part of the cornea is replaced it is known as lamellar keratoplasty. Keratoplasty simply means surgery to the cornea. The graft is taken from a recently deceased individual with no known diseases or other factors that may affect the chance of survival of the donated tissue or the health of the recipient.
Eye banks recover, prepare and deliver donated eyes for cornea transplants and research. The first successful cornea transplant was performed in 1905 and the first eye bank was founded in 1944. Currently, in the United States, eye banks provide tissue for over 80,000 cornea transplants each year to treat conditions such as keratoconus and corneal scarring. In some cases, the white of the eye (sclera) is used to surgically repair recipient eyes. Unlike other organs and tissues, there is an adequate supply of corneas for transplants in the United States, and excess tissue is exported internationally, where there are shortages in many countries, due to greater demand and a less-developed eye banking infrastructure.

A corneal ulcer, or ulcerative keratitis, is an inflammatory condition of the cornea involving loss of its outer layer. It is very common in dogs and is sometimes seen in cats. In veterinary medicine, the term corneal ulcer is a generic name for any condition involving the loss of the outer layer of the cornea, and as such is used to describe conditions with both inflammatory and traumatic causes.

Vernal keratoconjunctivitis (VKC) is a recurrent, bilateral, and self-limiting inflammation of conjunctiva, having a periodic seasonal incidence.

A pinguecula is a common type of conjunctival stromal degeneration in the eye. It appear as an elevated yellow-white plaque in the bulbar conjunctiva near to limbus. Calcification may also seen occasionally.
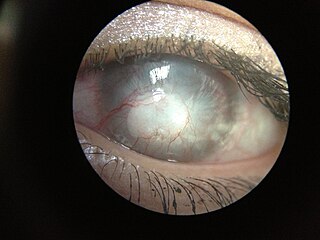
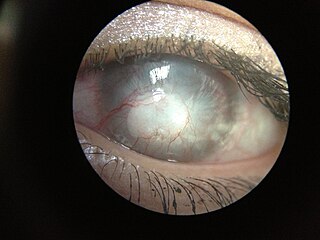
Corneal neovascularization (CNV) is the in-growth of new blood vessels from the pericorneal plexus into avascular corneal tissue as a result of oxygen deprivation. Maintaining avascularity of the corneal stroma is an important aspect of corneal pathophysiology as it is required for corneal transparency and optimal vision. A decrease in corneal transparency causes visual acuity deterioration. Corneal tissue is avascular in nature and the presence of vascularization, which can be deep or superficial, is always pathologically related.

Corneal ulcer is an inflammatory or, more seriously, infective condition of the cornea involving disruption of its epithelial layer with involvement of the corneal stroma. It is a common condition in humans particularly in the tropics and the agrarian societies. In developing countries, children afflicted by Vitamin A deficiency are at high risk for corneal ulcer and may become blind in both eyes, which may persist lifelong. In ophthalmology, a corneal ulcer usually refers to having an infectious cause while the term corneal abrasion refers more to physical abrasions.

Pellucid marginal degeneration (PMD), is a degenerative corneal condition, often confused with keratoconus. It typically presents with painless vision loss affecting both eyes. Rarely, it may cause acute vision loss with severe pain due to perforation of the cornea. It is typically characterized by a clear, bilateral thinning (ectasia) in the inferior and peripheral region of the cornea, although some cases affect only one eye. The cause of the disease remains unclear.

Pterygium refers to any winglike triangular membrane occurring in the neck, eyes, knees, elbows, ankles or digits.

Conjunctivochalasis is a common eye surface condition characterized by the presence of excess folds of the conjunctiva located between the globe of the eye and the eyelid margin.

Limbal stem cells, also known as corneal epithelial stem cells, are stem cells located in the basal epithelial layer of the corneal limbus. They form the border between the cornea and the sclera. Characteristics of limbal stem cells include a slow turnover rate, high proliferative potential, clonogenicity, expression of stem cell markers, as well as the ability to regenerate the entire corneal epithelium. Limbal stem cell proliferation has the role of maintaining the cornea; for example, by replacing cells that are lost via tears. Additionally, these cells also prevent the conjunctival epithelial cells from migrating onto the surface of the cornea.
Pre Descemet's endothelial keratoplasty (PDEK) is a kind of endothelial keratoplasty, where the pre descemet's layer (PDL) along with descemet's membrane (DM) and endothelium is transplanted. Conventionally in a corneal transplantation, doctors use a whole cornea or parts of the five layers of the cornea to perform correction surgeries. In May 2013, Dr Harminder Dua discovered a sixth layer between the stroma and the descemet membrane which was named after him as the Dua's layer. In the PDEK technique, doctors take the innermost two layers of the cornea, along with the Dua's layer and graft it in the patient's eye.
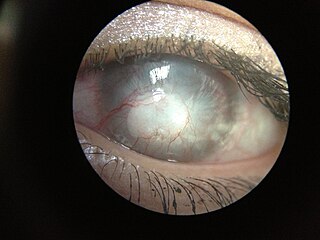
The human cornea is a transparent membrane which allows light to pass through it. The word corneal opacification literally means loss of normal transparency of cornea. The term corneal opacity is used particularly for the loss of transparency of cornea due to scarring. Transparency of the cornea is dependent on the uniform diameter and the regular spacing and arrangement of the collagen fibrils within the stroma. Alterations in the spacing of collagen fibrils in a variety of conditions including corneal edema, scars, and macular corneal dystrophy is clinically manifested as corneal opacity. The term "corneal blindness" is commonly used to describe blindness due to corneal opacity.
Pseudopterygium is the conjunctival adhesion to cornea caused by limbal or corneal inflammation or trauma. The pseudopterygium can be easily distinguished from pterygium by bowman's probe test. Because of the lack of adherence of pseudopterygium at every point, the probe can be passed beneath it at some point.
Exposure keratopathy is medical condition affecting the cornea of eyes. It can lead to corneal ulceration and permanent loss of vision due to corneal opacity.